Are you approaching the menopause or have you already hit it? Osteoporosis should be on your radar.
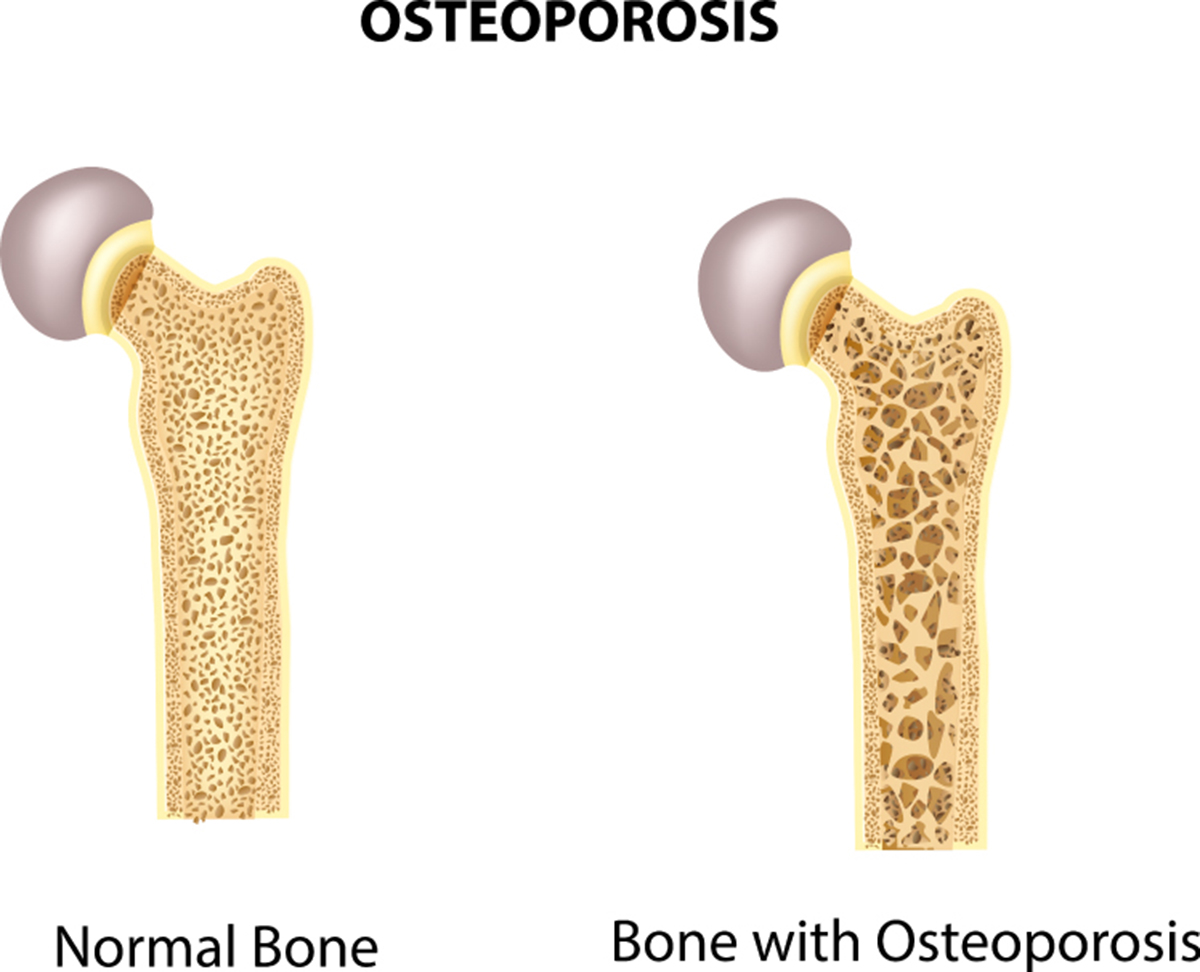
Osteoporosis — and condition in which you have brittle bones that have lost mass and strength — doesn't itself have any obvious symptoms, but it greatly increases your risk of fractures. Over 200 million people across the globe are thought to suffer from osteoporosis, and that includes more than 50 million older people in the US.
You should know that:
- More than 50 percent of women past the menopause will suffer a fracture linked to osteoporosis at some point in their lives
- Of these, a quarter will end up with a vertebral (spinal) deformity
- 15 percent of women will suffer a hip fracture after they enter the menopause
- Women have four times the risk of osteoporosis than men
Why does the menopause increase your risk of osteoporosis?
People under 30 tend to make more bone than they lose, helping them maintain strong bones that are less likely to break. That changes with age, and as early in life as 35, your body will lose more bone that it produces. This gradual decline in bone mass impacts women more than men, as they have thinner and lighter bones and are more likely to live longer.
Does osteoporosis come with any symptoms?
The loss of bone mass associated with osteoporosis doesn't itself have any symptoms, and that's part of what makes the condition so dangerous. Osteoporosis does, of course, place you at a higher risk of fractures — and it's when you break a bone, often after a fall, bump, or even a sudden wrong movement, that you're most likely to find out you have the condition. Osteoporosis can also lead to spinal deformities, and some people find out they have it after they or their doctor notice they're getting sorter, have a hunched posture, or suffer from chronic back pain.
Proactive steps to help prevent osteoporosis
There are plenty of things you can do to keep your bones strong and help prevent osteoporosis — and that starts with staying away from unhealthy habits. We all know that too much alcohol causes all sorts of adverse health outcomes, and that smoking does the same. You may not know, however, that nicotine lowers estrogen levels, and that drinking too much can do the same, along with lowering your calcium levels. Drink in moderation, then, and quit smoking if you're currently a nicotine addict.
In addition, diet and exercise can also go a long way toward decreasing your risk of osteoporosis.
Regular workouts for strong bones
Strength and resistance training, particularly, build stronger bones as well as stronger muscles. That doesn't mean you have to lift weights, though — walking, jogging, hiking, climbing, and even dancing are all examples of exercises that build strength and help prevent osteoporosis. Try to get at least 150 minutes worth of exercise in each week, and include cardio workouts as well. The increased flexibility exercise gives you may also lower your odds of falling, thereby making it less likely you'll end up with a fracture.
Pile on the calcium
Calcium is essential for strong bones, and you should try to get:
- At least 1,200 milligrams if you're aged 31 to 50
- Between 1,200 and 1,500 mg if you're over 50
You know where you can get calcium:
- Milk
- Other dairy products
- Seafood, like salmon and sardines
- Leafy greens like kale and broccoli
- Fortified foods like many cereals and orange juices
Are you getting enough vitamin D?
Vitamin D is special, in that sunlight is its main source — the majority of people can make enough vitamin D if they just spend half an hour or so in the day each day. Eggs, fatty fish, beef liver, and cheese are good food sources, along with products fortified with the vitamin. Because vitamin D plays a crucial role in calcium absorption and helps prevent osteoporosis, your doctor may also recommend you take a supplement. If you're 50 or above, you can take 400-2,000 IU of vitamin D per day, but don't exceed 10,000 IU.
Medications that can increase your risk of osteoporosis
Taking certain medications can cause more rapid loss of bone mass. These include:
- Some anticonvulsants
- Anticoagulants
- Thyroid medications
If you take any of these, talk to your doctor about how to reduce your risk of developing osteoporosis.
Treatment of osteoporosis
If you're diagnosed with osteoporosis, some of the same steps recommended for the prevention of the condition will be great for you, too — weight-bearing workouts, calcium, and vitamin D supplements are all important. Prescription medications are also available, however, and they include:
- Risedronate (Actonel, Atelvia)
- Alendronate (Fosamax)
- Ibandronate (Boniva)
- Raloxifene (Evista)
- Zoledronic acid (Reclast)
- Calcitonin (Fortical, Miacalcin)
- Estrogen replacement therapy
- Denosumab (Prolia) — a twice yearly treatment suitable for some people with good calcium levels
- Teriparatide (Forteo), an injection that promotes bone growth
What do you need to know about hormone replacement therapy and osteoporosis?
Hormone replacement therapy, in an osteoporosis-related context, may be recommended to women who:
- Went through the menopause early and thus have a lower lifetime exposure to estrogen
- Have a low bone mass, indicated by a bone density test
- Are at a higher risk of developing osteoporosis because they are especially petite, have a family history of the condition, or take medications that place them at a higher risk.
Are there any alternatives to HRT?
Yes, there are. If you decide hormone replacement therapy isn't right for you, or your doctor says it's not suitable for you, the following medications can also help you:
- Bisphosphonates, like Fosamax, Boniva, Actonel, and Atelvia slow the loss of bone mass
- Bisphosphonates can also be given through an IV once a year, in the form of Reclast
- Calcitonin, a natural hormone, sold under the brand names Fortical and Miacalcin
- Selective estrogen receptor modulator (SERMs), like Evista, behave like estrogen
- Prolia is an antibody therapy that is used twice a year
- Photo courtesy of SteadyHealth.com


Your thoughts on this