Table of Contents
Coronary artery disease is extremely common in adult diabetics. People who have diabetes are from two to eight times more likely to suffer clogged arteries than people of the same age, sex, and race who do not have diabetes.
Diabetics are also more likely than non-diabetics to have to deal with high cholesterol, high triglycerides, and high blood pressure. Even when diabetics keep one important risk factor in control, for instance, when they manage to maintain normal cholesterol levels, other risk factors take on added significance making heart attack and the need for cardiovascular intervention far greater.
Bypass and Stents in Treating Diabetic Coronary Artery Disease
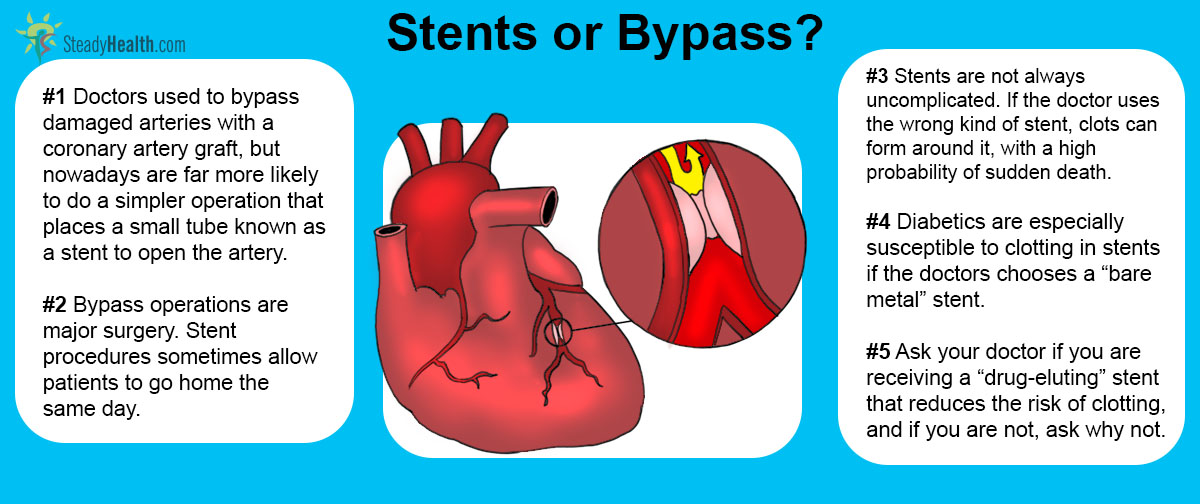
The two most common interventions for cardiovascular disease manifesting itself as atherosclerosis are coronary artery bypass grafting, more commonly referred to as bypass, and percutaneous coronary intervention, also known as coronary stenting.
In bypass, the surgeon harvests a vein from the leg, cracks open the chest, placing the patient in a heart-lung bypass machine and stopping the heart, and then sewing the vein around the area in which a coronary artery is blocked. Although less invasive versions of bypass exist, the procedure requires several hours under anesthesia and extensive trauma to the midsection of the body.
In coronary stenting, the surgeon opens a small incision, usually just 3 mm wide, into the femoral artery to run a catheter into the beating heart.
The surgeon then uses the catheter to introduce a metal coil into a segment of a coronary artery that has been damaged or closed by atherosclerosis, expanding the coil to keep the artery open. Stent procedures are performed with local anesthetic where they surgeon makes the incision into the femoral artery, and a sedative to keep the patient from moving around during the procedure. Some patients (including the author of this article) even watch the entire procedure on the doctor's fluoroscope.
Which Is Better for Diabetics, Bypass or Stent?
Cardiovascular surgeons usually prefer stent procedures to bypass. Every year about 350,000 Americans receive bypass surgery, while about 1 million receive stents. Both procedures are extremely expensive, about a quarter of a million dollars for an uncomplicated bypass and between $50,000 and $100,000 for a stent, but patients who receive stents often go home the next or even sometimes the same day, and patients who receive bypass often are in the hospital, or in and out of the hospital, for weeks.
Bypass surgeons in the 1990's typically earned over $1 million per year, but earn about $500,000 per year now. Surgeons specializing in stent placement, however, earn about the same amount.
See Also: Stent Or Bypass: Which Is Better For Treating Heart Disease In Diabetics?
In fact, some surgeons insist on bypass, rather than stents, for almost all their diabetic patients, despite the risks, costs, and length of hospitalization the bypass procedure requires. There are some very clear reasons why.
- Bangalore S, Toklu B, Feit F. Outcomes With Coronary Artery Bypass Graft Surgery Versus Percutaneous Coronary Intervention for Patients With Diabetes Mellitus: Can Newer Generation Drug-Eluting Stents Bridge the Gap? Circ Cardiovasc Interv. 2014 Jun 17. pii: CIRCINTERVENTIONS.114.001346. [Epub ahead of print] PMID: 24939927.
- Mindmap by steadyhealth.com
- Photo courtesy of Department of Foreign Affairs and Trade by Flickr : www.flickr.com/photos/dfataustralianaid/10711811543


Your thoughts on this