It is believed that after the age of 5, humans begin to develop plaques that ultimately form atherosclerosis. Western diets that are high in fats, red meats and carbohydrates accelerate this pathogenesis even faster and it explains why cardiovascular disease is one of the leading causes of death in North America. Thankfully, dietary modifications, exercise, and medications are three ways to make sure that we prevent long-term consequences like heart attacks from every occurring.
Unfortunately, many patients are not able to reverse this atherosclerosis process and it can build and build to the point of having a high degree of occlusion. If you are unfamiliar with the term, an occlusion is a medical term to describe vessel narrowing. The higher the degree of the occlusion, the more likely it is that blood will not be able to reach tissues. Without the sugars and oxygen of the blood reaching the tissue, it will die and will never be able to regrow. The manifestation of this would be an ischemic heart attack.

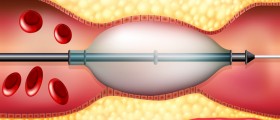
Thankfully, interventional cardiologists can step in to make sure that cardiac muscle is not irreparably damaged. They can do what is called percutaneous coronary intervention (PCI) to restore vascularization and reduce the occlusion. This is the preferred intervention in occlusion cases when patients are found to have blockages of greater than 70 percent. The cardiologist will use local anesthesia, insert a catheter and guide-wire into your coronary arteries, and then release a small metal coil (called a stent) to force the vessels to be wider. It is a very low-risk procedure, but unexpected bleeding or embolism are possible in rare cases. In most cases, patients will find immediate relief and they will be able to return home later that day. Patients are able to have multiple stents throughout their arteries and once resolved, the occlusion will be fixed for the rest of the patient's life.
Stents are the method of choice when you are dealing with a significant occlusion (greater than 70%) in one vessel but unfortunately, oftentimes, we have multiple blockages to worry about when we consider stenting patients. If a patient is found to have multiple occlusions in multiple areas, stents will no longer be as effective because the vessels may be too weak to support stents and this procedure could kill the patient. A coronary artery bypass graft (CABG) procedure is the treatment of choice in this circumstance. Surgeons will replace clogged arteries surrounding our hearts with veins harvested from our legs. These veins are clear of plaque and will last for 10 years on average, before another surgery would need to be considered.
If the occlusion has not yet reached 70%, we use a "watch and wait" approach in medicine. Patients are advised to radically alter their diets in order to stop making new plaques, take statin medication to remove some of the bad cholesterol that is flooding our arteries and to implement exercise regiments to improve our cardiovascular performance. In an ideal world, this occlusion will not progress and a patient will be able to live and healthy and happy life without the need for medical intervention.
The most important point to take from all of this is that it is much better for patients to routinely visit their physicians well before any of these symptoms occur. Patients should have annual blood tests after they turn 20 and family doctors should instruct patients on what to do well before chest pain or shortness of breath occur. Unfortunately, the fast-paced life of the modern world prevents patients from getting a chance to make it to a medical office and I routinely interview patients presenting with alarming symptoms with their last medical visit occurring 20 years prior. A minor inconvenience once a year is much more favorable to a life post-heart attack. Do what you can now to avoid anything like this from happening.
- www.ncbi.nlm.nih.gov/pubmed/19824825
- Photo courtesy of SteadyHealth