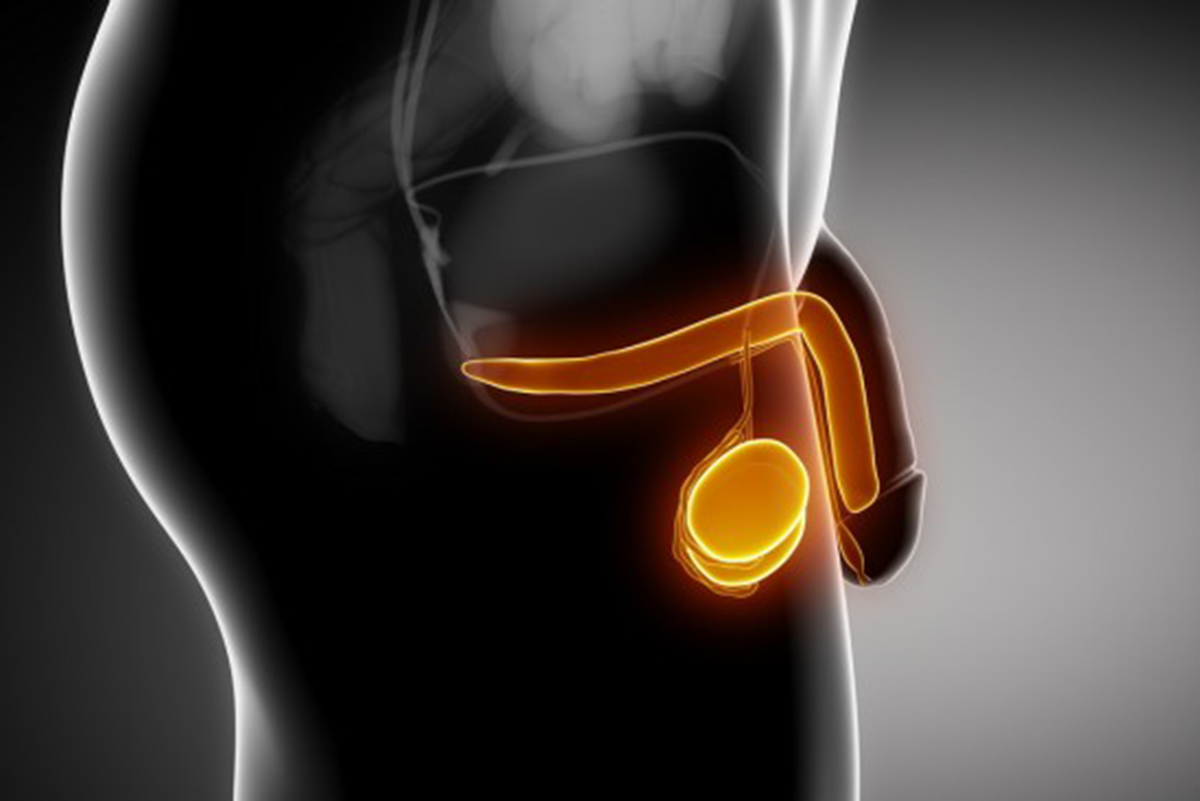
Testicles are normally positioned in scrotum, a bag-like formations just underneath the penis. They produce both male sex hormones and sperm cells. These hormones control the development of the reproductive organs and other male physical characteristics. As is the case with almost all other cancers, the cause of testicular cancer remains unknown. However, testicular cancer is highly treatable when diagnosed early. Regular testicular self-examination is essential for successful treatment.
Incidence of the condition
Caucasian males are at an increased risk of developing testicular cancer, as are men with a positive family history of the illness. Men whose testicles do not come down into the scrotum are also considered to be at great risk of cancer. Men with groin hernia, recurrent swelling of the testicles, or orchitis are all considered to be in a high–risk group.
Types of testicular cancer
There are two main types of testicular cancer: seminoma and teratoma. They have similar symptoms, but their histological structure is entirely different. Seminoma is made from a single type of cell, while teratoma consists of more then one type of cell.
There are two types of seminoma a swell, the classical type and the spermatocytic type. Over 95% of seminomas are classical. The average age of men with spermatocytic type of carcinoma is 55, which is almost 10 to 15 years older then the average age for all other types of testicular cancer.
There are also several other types of testicular cancer, such as embryonic carcinoma, yolk sac carcinoma, and choriocarcinomas, but they rarely occur .
Carcinoma that has spread on other parts of body is called invasive testicular carcinoma. The non-invasive form is called carcinoma in situ, or intratubular germ cell neoplasia.
Approximately 5 years is enough for the non-invasive form to transform into the invasive form. Detecting and diagnosing carcinoma in situ before it develops into cancer is difficult, because it causes virtually no symptoms.
Signs and symptoms of testicular cancer
Among many other symptoms, the most common one is a lump or swelling in one testicle. Other possible symptoms include:
- Tenderness or enlargement of tissue inside the testis
- Large amounts of fluid in the scrotum (hydrocele)
- A dull ache in the groin area or abdomen, especially the lower part
- Feelings of unusual heaviness in the scrotum
- Inexplicable fatigue
Of course, these symptoms are not a clear indication of testicular cancer in and of themselves. Most lumps in the scrotum should not be considered signs of testicular cancer at all.
Other diseases and conditions that can produce testicular lumps include
- Epididymitis- inflammation of epididymis
- Hydrocele
- Spermatocele
- Varicocele
- other kinds of benign scrotal masses
Self-examination for testicular cancer
Most testicular tumors are discovered by patients themselves - accidentally or while performing a self-examination. Regular testicular self examination, at least once a month, can literally save your life, because early diagnosis is essential for effective treatment.
Time required for complete self-examination is about 5 minutes.

You shouldn’t be alarmed if you notice a slight asymmetry, because it is quite normal for one testicle to hang lower than the other.
You should try to find a spermatic cord, called vas deferens. which goes from the top of the epididymis. It’s a smooth and firm tube. Then you can start the examination of the testicles. Ideally, they should be smooth, symmetric, and no lumps should be present in scrotum. Every testicle should be examined with both hands. The index and middle finger should be placed under the testicle with the thumbs placed on top. Then, just roll the testicle gently between the thumbs and fingers and seek for any abnormalities. Check the entire surface for hard, fixed areas, lumps and nodules. Most commonly, lumps are located in the sides of the testicles - very rarely they are found on top or under the testicle.
When you finish the examination of each testicle individually, look at both testicles at the same time. Put both testicles in your palm and check for asymmetry. Remember: slight asymmetry is completely normal, because one testicle is always a bit bigger and higher-positioned.
If you find any kind of lump, fluid, or significant asymmetry - seek medical help immediately. Although it doesn’t have to be a cancer, the abnormality may still benefit from early diagnosis and treatment.
Diagnosis
Only a physician can make a positive diagnosis. The final diagnosis can be set using several diagnostic tools, such as:
- Blood tests: These usually measure the presence of so-called tumor markers in the blood. They are a secure sign that there is some kind of cancer present in the body, Most common tumor markers are alpha-fetoprotein, beta-human Chorionic gonadotropin, and lactate dehydrogenase.
- Ultrasound: Ultrasound of the scrotum can show precisely if there is an abnormal mass in the testicle. This method can also rule out bacterial inflammation and other conditions unrelated to cancer.
- Biopsy: This is probably the best possible diagnostic tool. Histological structure examined this way is the secure sign of a cancer in the testicles. A clinical pathologist performs it, examining a tissue sample under a microscope.
Treatment of testicular cancer
Several types of treatments are commonly used for testicular cancer. The best method is determined depending on the type of cancer and how far it has spread.
There are several levels or stages of cancer spreading:
Stage I - cancer located only in testicles
Stage II - cancer has spread to regional lymph nodes
Stage III - cancer cells present in the abdomen
Stage IV - cancer has spread to other parts of the body
Testicular cancer is usually slow-growing, and tends to stay localized; in most cases it is diagnosed in stage 1 or 2.
Surgery: This is the most common and most invasive type of testicular cancer treatment. The operation of removing a testicle is called orchidectomy. All affected structures will also be removed, including regional lymph nodes. This operation is called retroperitoneal lymph node dissection and it could be far more complicated then the removal of testicle itself.
Because the cancer in most cases hits only one testicle, the removal does not affect a man's fertility or erectile ability later in life. There is even a synthetic protesis that can give a normal appearance, so, the only evidence left after the operation is the scar.
If both testicles are being removed, sperm can't be produced, and infertility is unavoidable. To circumvent this, a large amount of sperm could be deposited in a sperm bank for later use.
About 5% to 10% of patients have complications after the surgery, such as bowel obstruction or wound infection.
Radiation Therapy: This method uses high-energy rays to kill the rapidly growing cancer cells. This is considered “local therapy”, meaning it hits only the testicles. Unfortunatelt, these high-energy rays affect the normal as well as the cancerous cells. Possible side effects include fatigue, skin changes, loss of appetite, nausea, and diarrhea. Radiation will also adversely affect spermatogenesis in the healthy testicle (if there is one) for at least a year or two.
Chemotherapy: Strong anti-cancer medications are often used as the initial therapy of testicular cancer. The problem with this kind of therapy is that it represents a systemic type of therapy, which means these medications normally must travel all through the bloodstream and affect normal cells throughout the body. This can result in many possible side effects, such as coughing, shortness of breath, nausea, fatigue, diarrhea, hair loss, vomiting, fever, mouth sores, or skin rash. These mediations also kill the cells found in bone marrow, whose primary role is to produce and store blood cells.
- en.wikipedia.org/wiki/Testicular_cancer
- www.cancer.gov/cancertopics/pdq/treatment/testicular/Patient
- Photo by shutterstock.com

