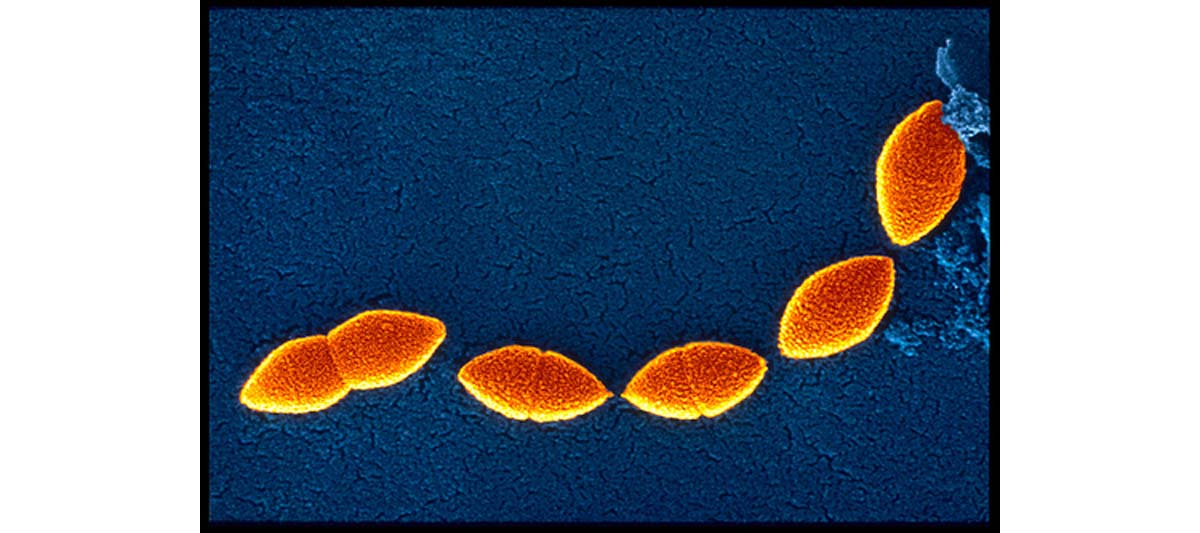
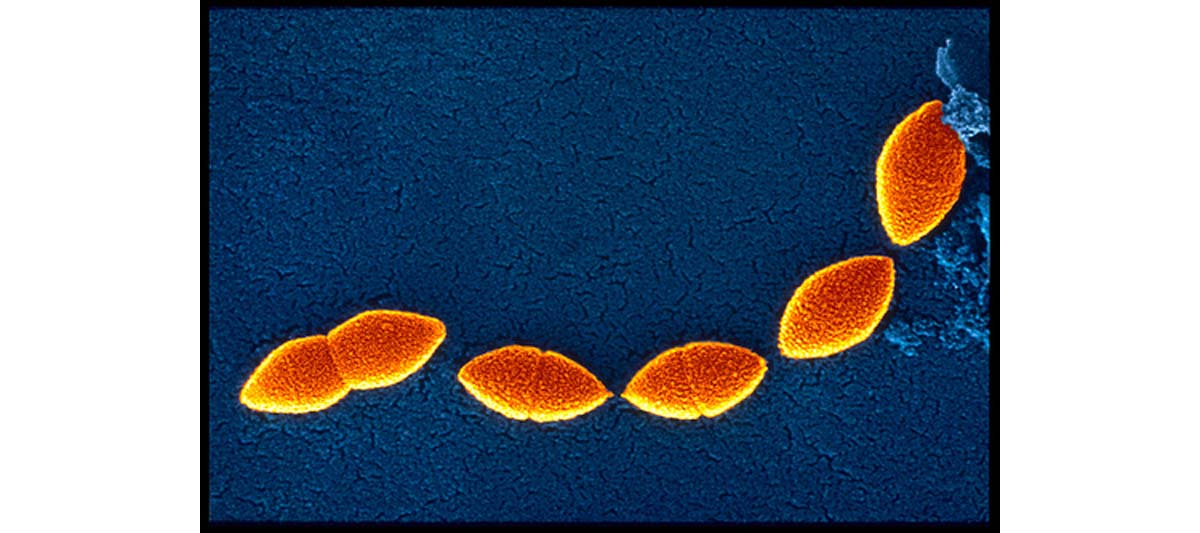
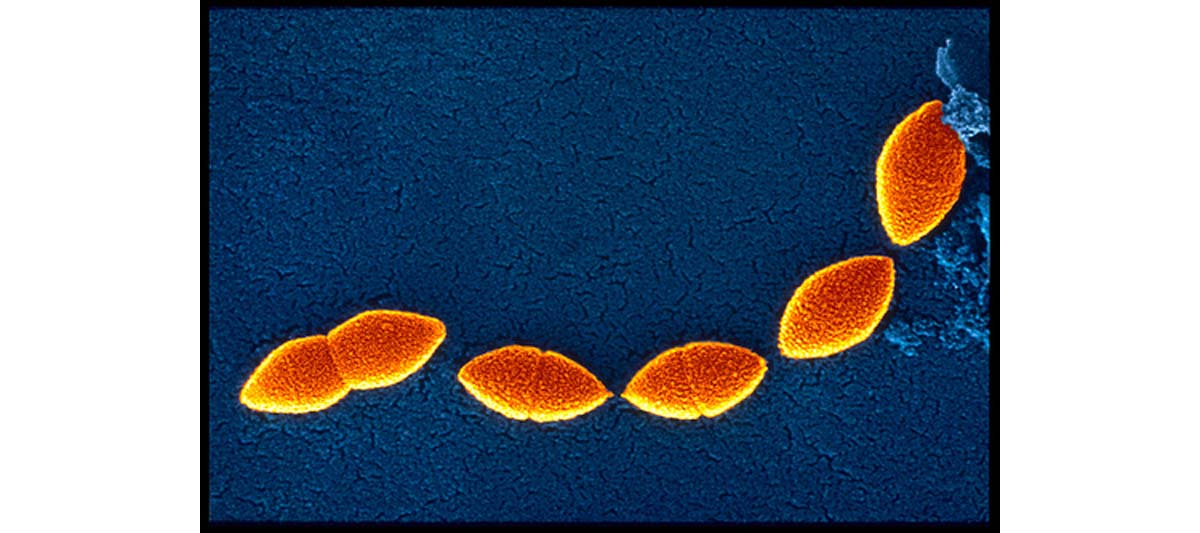
Septic shock is a potentially lethal drop in blood pressure due to the presence of bacteria in the blood. This condition, characterized by the presence of bacteria in blood, is also called the bacteremia.
It has been proven that bacterial toxins can, together with the immune system which responds to them, cause a dramatic drop in blood pressure, preventing the delivery of blood to the vital organs. What is the greatest danger of this septic shock? Well, experts are saying that septic shock can lead to multiple organ failure including respiratory failure, and may cause rapid death.
Possible causes and symptoms of septic shock

The most important fact is that when released in the bloodstream, these endotoxins are dangerous, because they become widely dispersed and affect the blood vessels themselves. It is normal that these arteries and the smaller arterioles open more widely in response, but at the same time, the walls of the blood vessels become leaky, allowing fluid to seep out into the tissues, lowering the amount of fluid left in circulation. It is logical to assume where all this leads! Several research studies done in the past have shown that this combination of increased system volume and decreased fluid causes a dramatic decrease in blood pressure and reduces the blood flow to the organs.
Under what circumstances does septic shock commonly occur?
Well, although there are no rules, most experts would say that the condition of septic shock is seen most often in patients with suppressed immune systems, and it is usually due to bacterial infections acquired during treatment at a hospital. How come? Well, there are two reasons.
First — the immune system is suppressed by the drugs used to treat cancer, autoimmune disorders, organ transplants, and diseases of immune deficiency such as AIDS, all of which are commonly used in hospitals. And second — the bacteria that are found in hospitals are much more resistant then the “usual” types found in other places!
Some research studies done on septic shock patients have shown that this syndrome most often occurs in menstruating women using highly absorbent tampons. How come? Well, it is easy to explain – these tampons, when left in place longer than other types; provide the perfect breeding ground for Staphylococcus bacteria, which may then enter the bloodstream through small tears in the vaginal wall.
Statistical data
· Frequency of septic shock
Several research studies carried out in the US have shown that more than 10 million patients who were diagnosed with sepsis were detected. This accounted for 1.3% of all hospitalizations. The overall incidence of sepsis increased 3-fold over this period of time from 83 cases per year per 100,000 population to 240 cases per year per 100,000 population.
Although mortality from sepsis is extremely frequent, the good thing is that these last couple of years, a reduction in hospital mortality rates for sepsis from 28 percent to 18 percent has been reported! Some large studies have proven a mortality rate for severe sepsis cases of anywhere from 30 to 50 percent, whereas simply meeting SIRS criteria carries a mortality of less than 10 percent.
· Race
It is important to point out that the incidence of sepsis is higher in the non-white population, with the incidence in black men being the highest at 331 cases per year per 100,000 population.
· Sex
Most of the research studies carried out on the topic have confirmed that men are more likely to develop sepsis.
· Age
Experts are saying that men tend to develop sepsis earlier in life than women.
Having said that, anyone, at any age, can develop septic shock.
Having said that, anyone, at any age, can develop septic shock.
Risk factors for developing septic shock
Risk factors for septic shock include:
· Diseases of the genitourinary system, biliary system, or intestinal system
· Recent infection
· Long-term use of antibiotics
· Recent surgery or another invasive medical procedure.
· Diabetes
· Diseases that weaken the immune system, such as AIDS
· Lymphoma
· Leukemia
Symptoms
Septic shock is a secondary state, which means that it is usually proceeded by bacteremia, which is characterized by the following symptoms:
· Fever
· Malaise
· Chills
· Nausea
Other symptoms of septic shock include:
· High or very low temperature, chills
· Lightheadedness
· Shortness of breath
· Heart palpitations
· Cool, pale extremities
· Restlessness, agitation, lethargy, or confusion
· A rapid heart rate
· Low blood pressure, especially when standing up
· Shallow, rapid breathing
· Decreased urination
· reddish patches in the skin
One big problem is that this septic shock syndrome may progress to cause "adult respiratory distress syndrome," or ARDS, which is an extremely dangerous condition because the fluid collects in the lungs, and breathing becomes very shallow and labored in these cases. Experts are saying that this condition may lead to ventilatory collapse, in which the patient can no longer breathe adequately without assistance — a life threatening condition!
Diagnosis of septic shock
How to recognize and diagnose the septic shock!? Like we have already mentioned in symptoms of the condition-the proper diagnosis of septic shock should be made by measuring blood pressure, heart rate, and respiration rate. Of course, parallel with all this should be searching for possible sources of infection. Most experts claim that the most precise diagnostic tool is simple blood cultures are done to determine the type of bacteria responsible for the bacteremia. If we look on the respiratory symptoms then we should know that the levels of oxygen, carbon dioxide, and acidity in the blood should also be monitored to assess changes in respiratory function.
Treatment
Like we have already mentioned, the severe sepsis is characterized by stimulation of a series of inflammatory cascades leading to extensive cardiovascular problems and the most obvious signs are hypotension due to vasoplegia, relative hypovolemia, and widespread dysfunction of the microvasculature. That’s why; the two major priorities in management of septic patients are
- To maintain delivery of oxygen to the tissues, by way of optimization of cardiac output and peripheral resistance, and
- To modulate the procoagulation response
Recommended antibiotics in septic shock
Suspected source
Recommended antibiotics
Pneumonia
Second- or third-generation cephalosporin plus macrolide (antipseudomonal beta lactam plus aminoglycoside if hospital-acquired)
Urinary tract
Ampicillin plus gentamicin (Garamycin) or third-generation cephalosporin
Skin or soft tissue
Nafcillin sodium (Nafcil, Nallpen, Unipen) (add metronidazole [Flagyl, Metro IV, Protostat] or clindamycin if anaerobic infection suspected)
Meningitis
Third-generation cephalosporin
Intra-abdominal
Third-generation cephalosporin plus metronidazole or clindamycin
Primary bacteremia
Ticarcillin and clavulanate potassium (Timentin) or piperacillin sodium and tazobactam sodium (Zosyn)
Possible complications
Significant complications from sepsis include:
· central nervous system dysfunction
· adult respiratory distress syndrome (ARDS)
· liver failure
· acute renal failure (ARF
· disseminated intravascular coagulation (DIC)
Prognosis
Every patient should know that the chanced for recovery from septic shock depend on several factors and the most important including:
· the degree of immuno-suppression of the patient
· underlying disease
· promptness of treatment,
· Type of bacteria responsible.
Prevention
Like we have already mentioned- several researches done in the past have shown that septic shock is most likely to develop in the hospital, since it follows infections which are the primary form of this condition. That’s why; in order to prevent this it is crucial to know that careful monitoring and early, aggressive therapy can minimize the possible likelihood of progression. It is logical to assume that the risk of developing septic shock can be minimized through treatment of underlying bacterial infections, and prompt attention to signs of bacteremia.

