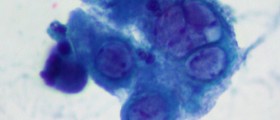
mode of infection of serratia in humans, mode of action,and their interaction with host immune response
Loading...
In the hospital, Serratia tends to colonize the respiratory and urinary tracts of adults, rather than the gastrointestinal tract.
Serratia causes about 2% of nosocomial infections of the bloodstream, lower respiratory tract, urinary tract, surgical wounds, and skin and soft tissues of adult patients. Outbreaks of S marcescens meningitis, wound infections, and arthritis have occurred in pediatric wards.
Serratia has caused endocarditis and osteomyelitis in people addicted to heroin.
Cases of arthritis resulting from Serratia infection are reported in outpatients who have received intraarticular injections.
The prevalence of Serratia in nosocomial infections is diminishing, but these bacteria still are able to cause hospital outbreaks, especially in intensive care units.
Crude mortality for nosocomial bloodstream infection with Serratia is 26%.
Mortality is high in patients with meningitis and endocarditis caused by Serratia infection.
S marcescens is naturally resistant to ampicillin, macrolides, and first-generation cephalosporins. In Taiwan, 92% of the strains are resistant to cefotaxime, but 99% are still susceptible to ceftazidime. Therapy for Serratia infections should include an aminoglycoside in addition to an antipseudomonal beta-lactam, as the single use of a beta-lactam can select for resistant mutants. Most strains are susceptible to amikacin, but reports indicate increasing resistance to gentamicin and tobramycin. Quinolones also are highly active against most strains. Definitive therapy should be based on the results of susceptibility testing because multiresistant strains are common.
Serratia causes about 2% of nosocomial infections of the bloodstream, lower respiratory tract, urinary tract, surgical wounds, and skin and soft tissues of adult patients. Outbreaks of S marcescens meningitis, wound infections, and arthritis have occurred in pediatric wards.
Serratia has caused endocarditis and osteomyelitis in people addicted to heroin.
Cases of arthritis resulting from Serratia infection are reported in outpatients who have received intraarticular injections.
The prevalence of Serratia in nosocomial infections is diminishing, but these bacteria still are able to cause hospital outbreaks, especially in intensive care units.
Crude mortality for nosocomial bloodstream infection with Serratia is 26%.
Mortality is high in patients with meningitis and endocarditis caused by Serratia infection.
S marcescens is naturally resistant to ampicillin, macrolides, and first-generation cephalosporins. In Taiwan, 92% of the strains are resistant to cefotaxime, but 99% are still susceptible to ceftazidime. Therapy for Serratia infections should include an aminoglycoside in addition to an antipseudomonal beta-lactam, as the single use of a beta-lactam can select for resistant mutants. Most strains are susceptible to amikacin, but reports indicate increasing resistance to gentamicin and tobramycin. Quinolones also are highly active against most strains. Definitive therapy should be based on the results of susceptibility testing because multiresistant strains are common.
Loading...