Chances Of conception
There is very little data in research which talks about conception following the removal of one ovary. It has mostly been studied in women with ovarian cancer or tumors which are not very aggressive. According to a study published in 2003 and 2007 in the European Journal of Gynecological Oncology, pregnancy rates, in women who have had removal of one ovary, have been reported as varying widely between 42 to 88 percent.
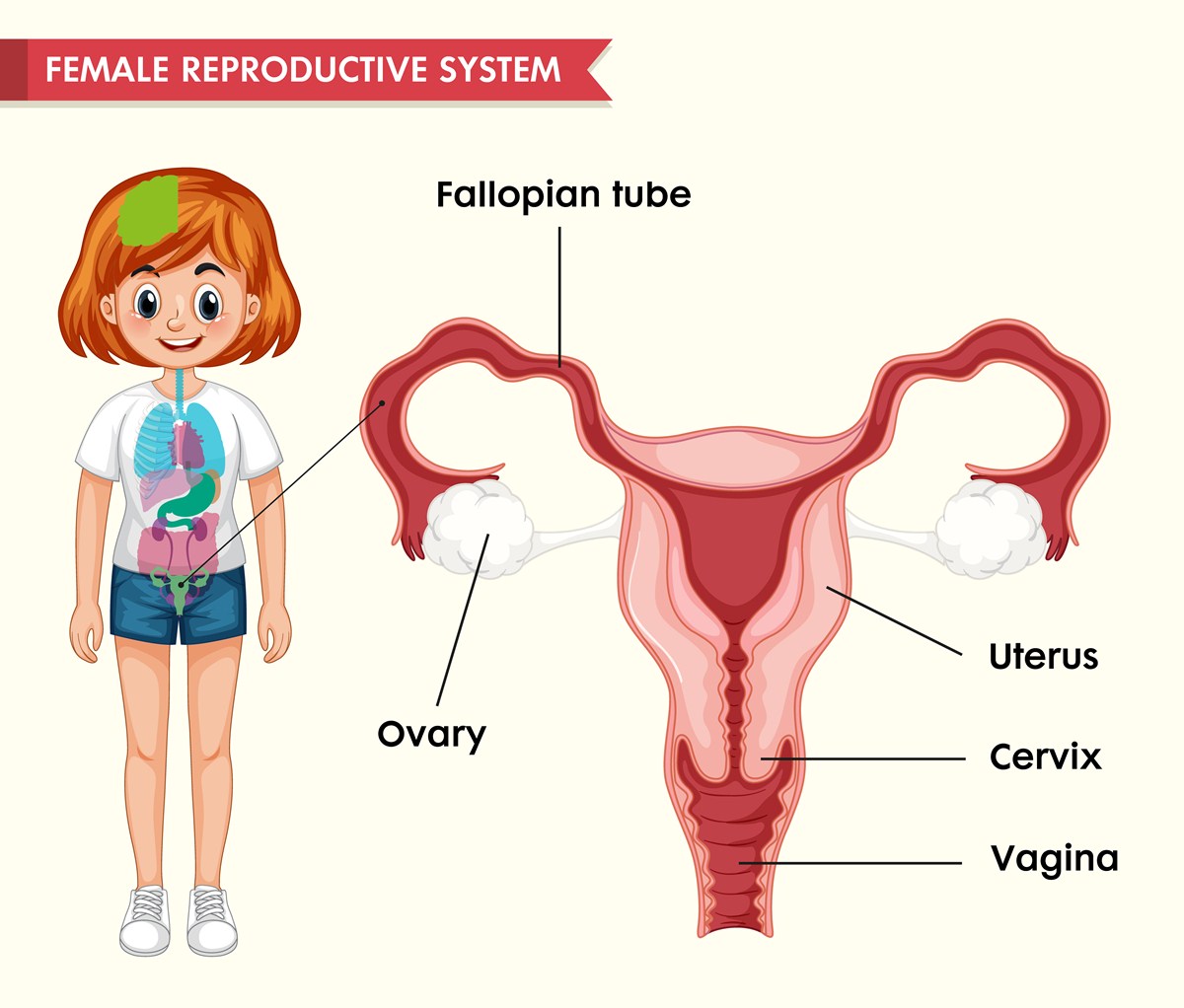
As you grow older, you have fewer and fewer follicles in your ovary. Follicles are the structural and functional units of the ovary, which bring about conception. This is the reason why, at menopause, the number of follicles have reached either a zero state or a state in which even the follicles which are remaining are not able to function fully.
Now, there is reason to believe that a younger woman who has her ovaries removed has a higher chance of conception just because of the fact that she the number of active follicles in her ovary are more than someone who is older than her. Younger women should have lots of follicles in their remaining ovary, which makes conception highly likely.
In Vitro fertilization(IVF): Now, regarding how these women do with in vitro fertilization, the answer we get from research studies is very mixed, which means that it was not clear whether in vitro fertilization would be successful or not. This is according to a research study published in 1999.
Additional Hormones: Patients will not need additional hormones, unless they have additional symptoms. These symptoms could be absence of menstruation or infrequent menstruation. Infrequent menstrual cycles are practically considered when menstrual cycles last longer than six weeks. If you have these symptoms of absence of menstruation or infrequent menstruation, you need to visit your gynecologist.
Your gynecologist might, then, prescribe hormonal supplements in a dose and frequency that will mimic the normal production of these hormones by the ovary. These are the symptoms of premature ovarian failure. In premature ovarian failure, the ovarian follicles have been damaged to such an extent by the disease and the surgery, that it is almost like having menopause.
Elective oophorectomy or conservation at the time of hysterectomy(removal of uterus)
The traditional way has been to remove both ovaries when women are getting their uterus removed. However, currently, the recommendation is to preserve the ovaries during removal of uterus, if the woman has no increased risk of ovarian cancer. Oophorectomy has been shown to reduce the risk of ovarian cancer and a probable reduction in the risk of breast cancer who had their ovaries removed premenopausally. However, removal of ovaries has been shown to increase the long-term mortality and cardiovascular risk in women under the age of 50 who do not take estrogen therapy.
Therefore, for women who undergo hysterectomy for non-cancer related causes and who do not have suspicious ovarian disease or familial cancer tendencies, ovarian conservation during the time of hysterectomy has been suggested.
Removal of ovaries can be reasonable for those above 51 or for women who place a higher priority on cancer prevention than on potential risks of long-term mortality or cardiovascular disease.
- Eur J Gynaecol Oncol. 2003
- Eur J Obstet Gynecol Reprod Biol. 2007
- Hum Reprod Update. 1999
- Photo courtesy of SteadyHealth