I had my TC 5 years ago. I was in the hospital for 11 days with no complications other than the pain of the air in the abdomen going into my neck on day 10 but that was over pretty quickly. The more you walk after surgery the better off you will be. The NG tube I woke with was uncomfortable after about the 2nd or 3rd day. I begged my doc to remove and after he all but begged to leave it for one more day, he agreed to remove and sure as he told me I started vomiting. That also didn't last too long. Good news is that it has been 5 years and I have not vomited since. I wounder if this is something that happens with all total coletomy patients or just me. Anyway. It was the best thing I ever did for my own health. I can eat the same as I did before. I will tell you that I still get stopped up if I eat a salad. I think this is just me but even after five years I am still scared of getting constipated again and with me it does happen occasionally. Probably something I am eating causing a blockage, but it never last more than a day. and 1 tbsp of mile of magnesia goes a long way. Good luck with your surgery and remember that it takes a good 2 months to totally feel like you are back to normal. You will lose a substantial amount of weight during the early process but you will easily gain it all back as soon as you start eating again. I had severe hemorrhoids before my colon surgery due to constipation and 4 weeks after my surgery my local doctor decided it was best it he removed them. Never let anyone talk you into anything like this right after colon surgery. 1-12 BM's a day after hemorrhoid surgery is literally like being tortured. That is the worst pain I have ever experienced and I am a mother of 4.
Loading...
I think everyone's experience is so different (and the bad experiences are sometimes the ones you will hear the most about) that it's hard to know exactly what to expect. And probably the best advice during recovery is to listen to your body. My total colectomy was around 1.5 years ago and I'm doing awesome! I was keeping-down liquids the day after surgery and 36 hours after had an accidental BM while sleeping (which was so exciting that I wasn't even embarrassed). Despite being up and about soon after surgery, by the evening of the 2nd day after surgery I suddenly ended-up with severe ileus (where nothing is getting through the small intestine, common after abdominal surgeries and often but not always preventable by getting out of bed early) in which I was extremely bloated, severe gas pain, horrible nausea and liters of bilious vomiting requiring NG placement on suction and rectal tube placement for the next 5 days or so. I kept trying to walk despite the pain to get things moving. Then after around 5 more days things suddenly completely turned around (literally and figuratively) and I was able to eat, had NO pain, and actually felt better than I had in 3 years! I was having probably 12-15 BMs a day at that point but I certainly preferred this to having 1 BM every 12-15 days!!!
I was in the hospital 10 days total (would have been much less except for that ileus issue partway through). By around 2.5 weeks after surgery I was jogging a couple of miles a day (on the treadmill - needed a bathroom nearby), whereas in the years prior to the surgery walking short distances was a struggle. I could eat spicy foods without painful reflux. Gradually the number of BMs per day decreased and became generally (but not always) predictable based on timing of meals. Now I range from 2-6 and they are watery but unlike the diarrhea that accompanies a GI bug these are generally not super urgent or accompanied by cramping. Fiber supplements can help decrease the frequency but personally they make me feel kind-of distended/backed-up and I find I'm most comfortable if having 3-4 BMs/day. I still have unpredictable BM incidents from time to time requiring me to quickly leave meetings, etc. and unfortunately most of the people I work with (despite being other doctors!) are not very understanding but whenever I'm having a "crappy" day (bad pun intended!) I just remind myself how much better I'm doing overall than prior to my surgery and how I truly feel like all the ups/downs of my own medical experiences are making me a better doctor.
I am not vegetarian but have never eaten very much meat. My greatest frustration as far as diet is that I can no longer tolerate large salads or large amounts of raw produce, especially vegetables, in general. This is frustrating because I've never gotten into the habit of doing much cooking so raw veggies/salads were a huge part of my diet. I know others post-colectomy who have had this problem and lots of others who have not. I try to eat more cooked food now.
My advice to anyone as far as immediate post-op that I wish someone would have emphasized to me and that I now try to emphasize to my own patients is about how to prevent/cope with ileus (while also realizing that of course this won't apply exactly to every patient). I'm willing to guess that you likely have a high pain tolerance at this point but even so the gas-type pain can be absolutely excruciating (and much more than any incisional pain) and the last thing you may feel like doing is walking around but forcing oneself to do this can be crucial in preventing and helping resolve ileus. Unfortunately doesn't always work but can make a big difference. The second thing is that in many people the pain medications (even the strongest narcotics) don't do anything for this type of pain; likewise the antihistamines used for nausea (e.g. Compazine, Promethazine) aren't always particularly helpful with ileus-related nausea. If you end-up with ileus I would suggest trying these meds and if they help then great - obviously being less nauseated and in less pain will help with getting up and walking. However, if they don't seem to be making a difference anyway stop taking them! Both categories actually have slowing effects in the GI tract and can make things worse in that sense. But, again, as I said if these meds are helping with symptoms then taking them is worth this side effect if it helps you get out of bed and walking around more. It's a balancing act!
Sorry this is so long but hopefully it answers some of your questions! Good luck!!
Loading...
Thank you for taking the time to post your story. I am going through the consideration process now of having my colon removed due to Colonic Interia. I am trying to weigh continuing to take multiple laxatives and prescriptions daily and being up most of each night sick with pain, bloating, and having to go to the bathroom.... with having the surgery. The idea of not having to take all these meds and being able to eat like others and actually sleep most of the night is very appealing. However, I'm concerned about how "intrusive" the urge to go will be while I'm trying to work a fairly demanding job.
Obviously, the surgery is permanent, and I have gone back and forth about it for a week now. I know the devil I have which I can control by taking more or less laxatives, and I'm concerned about the devil I don't know (and not having as much control of urges).
Anyone with experience with this surgery's input/ thoughts is most appreciated! I've lived with this for approx 15 years, but it has only gotten worse.
Loading...
I would SERIOUSLY get 2-3 opinions BEFORE having your surgery! I am speaking from vast experience. Not only will I detail my horror story here I am willing to give you my phone number if you would like to speak with me if you read my reply. I had my gall bladder removed at the age of 17 due to GI problems. things continued to be a problem over the years. I took OTC antacids etc. Throughout my 20's I yo-yo dieted as my weight would go up & down never really understanding my constipation issues or stomach pains. Dr's never gave a clear answer. After having my child at 30 I realized the pain was too much and none of the prescriptions were working. In 2009 I saw my primary care Dr. because I hadn't had a bowel movement for 28 days! I then saw a specialist. It took 2 months before surgery. By then I was septic. All the tests they had run did no good at all, they punctured a hole in the lining of my stomach during surgery and my entire system became infected. My appendix had to be removed! I then had to have an emergency illeostomy which was not part of the original surgery. I had a 10% chance of survival. I was in ICU for 22 days. I wore that colostomy bag for 8 months before it was reversed. To this day I have a hard time eating and I still go to the bathroom 10-15 times a day. February 15th of this year I was rushed to the ER because I thought I had food poisoning but oh no, I had a hole in my esophagus. It was slowly leaking food into my stomach. I hadn't been able to put weight on in the last 3 years since my surgery. this was the reason. A hernia! I was septic again. My white blood count was only 2500. I could have died anytime. Since that surgery I have somehow put 40 pounds on in 9 short months! How? I have no idea. I have one heck of an absorption problem though. I drink water all day yet I am always dehydrated. I am tired. I am hungry. I am always in the bathroom. I am dizzy. I throw up. My Dr calls it dumping syndrome. It is a nightmare. I can not work. I am depressed. My family worries about my all of the time. Please get a second opinion! Yours truly, Sarah J
Loading...
Oh my gosh, Sarah, I'm so sorry to hear about all you've gone through! It sounds like a nightmare that won't end... I think your advice to get second opinions is good, and I requested authorization from my insurance company last week. I am so worried that the effects after surgery will be worse than they are now. I know the devil I have now, but who knows post surgery?I worry about the urgency/ lack of control/ not being able to eat some of the same things I do... I already have a lot of food allergies, so to further limit what I can eat would really be a problem.I also have to move right after recovery, so I won't have much of a support system nearby... and my job will require me to travel a fair amount. Just so conflicted about whether to have the surgery or not.I will get a second opinion though - thank you and I wish you all the best in feeling better!
Loading...
I had a sub total colectomy in 1994, went back a few times adhesions, kink in the bowel, and more removal of the large intestine, my one stay was for almost 3 weeks..I do not have a stoma. My doctor told me to eat several times a day, but just small meals. I have heard stories about eating fibre and not eating fibre, so I think it is different for everyone. In all fairness, I think you should get 2nd or 3rd opinions, I would just assume that because you are not eating enough that you have grown weak, as from what you have said you eat, no one can survive on that amount of food and be "healthy". If you were in SA I would have recommended my Doctor Charles Treurnicht, the man is a genius !!! I'm 3x older than you, and I am going to have my 60th on the 8th December 2013, a lot of people thought I was a gonner, those years back. There is hope, keep on believing, please, you are so young, keep on trying until you get a doctor/specialist that can help you. I don't think you should be suffering pain every time you eat! I'm sorry I can't help you, I'm just trying to tell you there is help out there, you have to get a specialist's help, you have lost too much weight as it is. If you were a super athletic, you are a fighter, so keep on fighting until you get the correct help you need. Best of luck and blessings from God. Marilyn South Africa
Loading...
Cera, I had same thing done and terrible repercussions. However, I am still alive, if still very miserable. A friend of mine had this surgery done on Sept 17, 2013 and died in ICU the first week of December, in an eerily similar story to yours.
Oh, gosh, when my gastro said he was just going to "cut that bad part out and you'll be fine" I was in so much pain I couldn't sign the consent forms soon enough. 13 years ago and miserable almost every single day. Gas pain, bloating, constant bms, watching every single thing I eat because I know how much it is going to hurt later;
I tried to talk her out of the surgery. I told her it probably wouldn't fix it and she would be trading one set of issues for another. But I never, never really thought she would die. But she did. Sepsis, dehydration.
So I have to vote a big no to this surgery even though it seems like a magic cure.
I also suffer from malabsorption and have to have iron infusions and blood transfusion three or four times a year.
There has GOT to be a better solution.
Loading...
I had my total colectomy in Dec of 2001 after a large bowel obstruction in Sept of 2001 that almost took my life. Up until then, the dr's all told me to drink more water and eat more fiber. Yeah, cause that solves everything. I hate to say it, but i still get constipated. I think for me, my small bowels have slowed down as well. It has created a lot of issues for me over the years, but i have to say, I would do it all over again. I have had bowel obstructions from adhesions, hernia surgerys from my colostomy site, adhesion removal from all the surgeries, but again, I would do it all over again. I have a good Gastro DR, but to be honest, I learn alot by trial and error. I stick to the low fiber diet. Small meals and if i feel sluggish, i drink plum juice. For the first 3 years, i was great. I couldnt drink juice because it would go right through me. But over the years, my small bowels have slowed down. I take Amitiza, but if i drink orange juice all day, it works better. If it gets bad, i will do plum juice (so much better than prune juice). I have a great support system at home and at work. I dont get to take a lot of vacations cause i end up using all my leave for dr's appointments or surgerys. I have had 5 just in the last 3 years. But, it is still worth it. They say eventually i will need a colostomy bag if my small bowels totally shut down, but i will do what i can to keep that from happening. Really, if it does, its not the end of the world. I had one for 4 months after my first blockage and there are worse things that could happen. I could have died. :)
Loading...
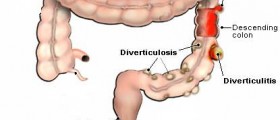
i really appreciate your telling about your experience. i have had constipation issues my whole life. as of 2009, i had to start taking pain medications for my back so of course they blamed it on that. after trying all the different medication they would throw at me ,diets etc... i would have to take 3 then 2 dulcolax for 3 days with some relief and then do it all over again in a week. i knew that taking them constantly wasn't good for me but as you said, i am not being taken seriously. the last colonoscopy i had showed that i had inside hemmoroids (wonder why) and diverticuli. sent me on my way with a new diet .... a year has gone by ( back to using the dulcolax ). i have an appt. next week but this time i have something new to tell him-- i have ribbon stools. really tired of this. being so uncomfortable and i pain,bloated as heck,unable to fit in my clothes and unable to have company.... i hope it works out for you hon !
Loading...
At 9-month follow-up, I wonder if subtotal colectomy with ileorectal anastomosis was the right procedure of choice for my intractable slow-transit constipation. Surely, I am not constipated anymore/ my bowel-movement frequency has changed (diarrhea, more than 7 voids per day), but the functional outcomes remain the same: abdominal pain, bloating, digestive trouble and nausea. I hoped that after this huge decision of the surgery (that many of you know how huge this is) I would finally be relieved and I was excited to have a new life.. but I don't! Post-operatively, I am on a strict diet and I have followed various pharmacologic therapies, homeopathy, yoga and acupuncture. Once again, the conservative approach seems to be ineffective in correcting the abnormalities. My GI doctor told me about something I had never heard before: Recent studies strongly indicate that a dysfunctional neuroendocrine system may contribute to the etiopathology of colonic inertia. In this case, colectomy can not be an effective treatment (Of course, my large intestine was almost dead and had to be removed, and therefore the solution was the surgery). When treating chronic painful conditions, it is of the utmost importance to establish a good doctor-patient relationship. Since my 20's I have seen many doctors that didn't take me seriously. I trust my doctor. However, I don't like the new therapy he proposed. The strategy to correct the neuronal alterations and “re-build a new brain” may involve combinations of multiple antidepressants and a variety of psychotropic medications -antipsychotics (antidepressants alone may be inadequate) for a long-long time. I know that antipsychotics are used for non-psychiatric medical disorders too, but still.. it is hard for me to perform this technique until more convincing data has been published. On the other hand, maybe this is the final step for having the quality of life that I 've been dreaming of.. Does anybody know if this strategy has been formally evaluated for the treatment of my situation?
Loading...
First, I am so sorry for your loss. TY for reading my post. My newest gastro problem is a new small bowel obstruction. I've gained in excess of 40 pounds since my last surgery. I see yet a new specialist in the end of Jan. It just doesn't stop.
Loading...
Loading...
Loading...