Hi Amberjoy
I would suggest that your doctor will continue you on non weight bearing for at least another 3 weeks so you'll have done a total of 8 weeks non weightbearing.You may have to keep the cast, although if you ask (you may have to plead!!) he/she may give you a camwalker boot, as long as you promise you won't walk on it. These are great because you can start to rehab your ankle by rotating it around a bit. You can also wash your leg! After 8 weeks non weight bearing, if all looks good on the xrays, you may be able to walk on it in the boot. This will be for another 4 to 6 weeks. During this time you will begin to rehab your ankle and leg. Some doctors are more conservative than this and will leave you non weight bearing for 10 to 12 weeks. Listen to your doctor but I would suggest definitely non weightbearing for at least 6 weeks and no less! Since you did not have a fusion, it seems that a lot of doctors like to remove the hardware before you do any walking without the boot to prevent breakage. Others like to keep the hardware in for at least 6 months or longer. You'll have to ask your doctor what they are planning for you. Make sure you do, as it is a good idea to know what is ahead of you so you can prepare yourself mentally.
I hope this info helps. You can write again when you reach the next phase and I will tell you what we went through then.
Gymnastics Mom
I would suggest that your doctor will continue you on non weight bearing for at least another 3 weeks so you'll have done a total of 8 weeks non weightbearing.You may have to keep the cast, although if you ask (you may have to plead!!) he/she may give you a camwalker boot, as long as you promise you won't walk on it. These are great because you can start to rehab your ankle by rotating it around a bit. You can also wash your leg! After 8 weeks non weight bearing, if all looks good on the xrays, you may be able to walk on it in the boot. This will be for another 4 to 6 weeks. During this time you will begin to rehab your ankle and leg. Some doctors are more conservative than this and will leave you non weight bearing for 10 to 12 weeks. Listen to your doctor but I would suggest definitely non weightbearing for at least 6 weeks and no less! Since you did not have a fusion, it seems that a lot of doctors like to remove the hardware before you do any walking without the boot to prevent breakage. Others like to keep the hardware in for at least 6 months or longer. You'll have to ask your doctor what they are planning for you. Make sure you do, as it is a good idea to know what is ahead of you so you can prepare yourself mentally.
I hope this info helps. You can write again when you reach the next phase and I will tell you what we went through then.
Gymnastics Mom
Loading...
Well, I saw the Dr. today. First they did x-rays of my foot, wow what a mess of metal it is! Nine screws, 1 plate, and 2 pins! He said it is a very severe injury and that all of my bones were dislocated as well as three of my metatarsals crushed. All because of a 2 inch deep divet in my front lawn!! Anyways, when he asked me how I was doing I told him I would be a lot better once he took these pins out...unfortnately he did not take them out and I have to wait another three weeks with them in as well as remain NWB during that time. He also said that most if not all of the screws will remain in my foot for 1 1/2 years...is that normal??
On a positive note, he did give me the go ahead to wear a Cam boot and I get to go back to work 4 hours a day! It will be nice to get back to some normalcy of my day. When I got home I got in the bath and soaked my foot. It was absolutely disgusting to think, and see that you are shedding that much skin in 6 weeks. It definitely feel better to have msot of it off though and to be able to massage my foot and move my ankle. Now it's on to going back work and back to getting my two year old up and dressed in the morning...should be exciting!
On a positive note, he did give me the go ahead to wear a Cam boot and I get to go back to work 4 hours a day! It will be nice to get back to some normalcy of my day. When I got home I got in the bath and soaked my foot. It was absolutely disgusting to think, and see that you are shedding that much skin in 6 weeks. It definitely feel better to have msot of it off though and to be able to massage my foot and move my ankle. Now it's on to going back work and back to getting my two year old up and dressed in the morning...should be exciting!
Loading...
When I was diagnosed with a lisfranc injury last year, I read so many disheartening stories in this forum that I told myself if I got better I must revisit to tell my story. At that time I felt I lost all hope of ever walking normal again. I really wished more people who recovered fully had shared their stories.
I fell down the stairs on 3 August 2008 and landed awkwardly on my left foot. I was 17 weeks pregnant at that time. I was not able to walk on the foot at all after the fall and was sent straight to emergency. By the time they saw me my foot was so swollen and totally bruised. I told the docs I did not want to take an xray at that time since I was pregnant. The doctors said ok and told me to come back in 3 days if it was still swollen. Three days later, had my foot inspected by a GP and was referred to an orthopedic surgeon. In the end consulted 3 orthopaedic surgeons who all said the same thing - I had a lisfranc dislocation on the 1st and 2nd met which would require surgery ASAP.
I had my surgery on 20th August, stayed one night at the hospital. I had 3 screws put in which my doc said will be taken off after one year. The pain from this surgery was the worst. I woke up in the middle of the night in so much pain, but was told to go easy on the pain killers because of the pregnancy. The pain came on and off afterwards and lasted about 2 weeks.
Two weeks later I had the stitches removed and was put on a non-weight bearing cast for 6 weeks. After that it was followed by 4 weeks weight bearing with the boot. I started physio 2 weeks after I was out of the boot, twice a week for about 2 months.
I was off work for a whole month and working from home the next month. The hardest part of this injury was the uncertainty of the outcome esp after having to go through the pain and difficulty of non weight bearing. Once I started weight bearing I was still unsure as the swelling was vicious, though partly could have been due to my pregnancy.
I am now 10 days post screw removal surgery. The surgery was nothing compared to the first one, I was walking out of the hospital on my own. I am still waiting for the bandage to be removed but already can feel a lot more movement when I walk. I am now walking as normal as I can remember and am able to do long walks without pain.
These are some important things that I wished someone had pointed out to me when I suffered the injury:
• Get a good orthopedic surgeon specializing in foot and ankle, one who knows and has done such surgery
• Don’t delay the surgery if it’s required. I healed well because surgery was done without delay and I did not walk on the bad foot at all after the fall
• Once you start walking, try and walk as normal as you can even though you are slow. This will ensure you don’t pick up any bad habits
• Massage your foot whenever possible, I did this almost daily with some Chinese ointment to improve circulation
I am more than happy to answer your questions if you have any. Hope this helps :-)
I fell down the stairs on 3 August 2008 and landed awkwardly on my left foot. I was 17 weeks pregnant at that time. I was not able to walk on the foot at all after the fall and was sent straight to emergency. By the time they saw me my foot was so swollen and totally bruised. I told the docs I did not want to take an xray at that time since I was pregnant. The doctors said ok and told me to come back in 3 days if it was still swollen. Three days later, had my foot inspected by a GP and was referred to an orthopedic surgeon. In the end consulted 3 orthopaedic surgeons who all said the same thing - I had a lisfranc dislocation on the 1st and 2nd met which would require surgery ASAP.
I had my surgery on 20th August, stayed one night at the hospital. I had 3 screws put in which my doc said will be taken off after one year. The pain from this surgery was the worst. I woke up in the middle of the night in so much pain, but was told to go easy on the pain killers because of the pregnancy. The pain came on and off afterwards and lasted about 2 weeks.
Two weeks later I had the stitches removed and was put on a non-weight bearing cast for 6 weeks. After that it was followed by 4 weeks weight bearing with the boot. I started physio 2 weeks after I was out of the boot, twice a week for about 2 months.
I was off work for a whole month and working from home the next month. The hardest part of this injury was the uncertainty of the outcome esp after having to go through the pain and difficulty of non weight bearing. Once I started weight bearing I was still unsure as the swelling was vicious, though partly could have been due to my pregnancy.
I am now 10 days post screw removal surgery. The surgery was nothing compared to the first one, I was walking out of the hospital on my own. I am still waiting for the bandage to be removed but already can feel a lot more movement when I walk. I am now walking as normal as I can remember and am able to do long walks without pain.
These are some important things that I wished someone had pointed out to me when I suffered the injury:
• Get a good orthopedic surgeon specializing in foot and ankle, one who knows and has done such surgery
• Don’t delay the surgery if it’s required. I healed well because surgery was done without delay and I did not walk on the bad foot at all after the fall
• Once you start walking, try and walk as normal as you can even though you are slow. This will ensure you don’t pick up any bad habits
• Massage your foot whenever possible, I did this almost daily with some Chinese ointment to improve circulation
I am more than happy to answer your questions if you have any. Hope this helps :-)
Loading...
Hello,
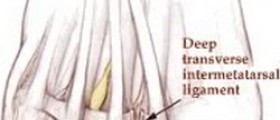
My very sports oriented 18 year old daughter suffered a Lisfranc injury - surgery was done within 18 hours through the Emergency - she has three screws [one from her 1st MT to 1st Cuneiform, one from her 2nd MT to 2nd Cuneiform, and I believe one crosswise]. Not completely sure about the direction of the third screw as I was told where they would put the first two before surgery and that they may need to pin the other 3 MT, however I missed the surgeon before she was released from hospital as he was an Emergency call-in Orthopedic Surgeon but as she is considered an adult he did speak to her post-op. So he did tell her about the third screw, and that they did not use any pins. I will know more in a week at her first Ortho appointment [which will be 17 days post-op].
She's a very active student who is getting around okay in the post-op bindings with her crutches. I do have some concerns and questions.
1. She experiences alot of pain when she gets up from a resting position with her foot up, is this due to the fluids/blood rushing into the foot? It tends to ease off once she's up for a bit, but alot of throbbing at first.
2. She's very active in the sense that she has to get around to classes, just how much should she be resting the foot? And when they say put the foot up, must it be above heart level, or is up on a pillow sufficient?
3. With all of the post-op bindings, how would we tell if there were an infection? [She was given a course of IV antibiotics after surgery and prior to leaving the hospital]. I noticed [near her toes] a mark that resembled a strawberry birth mark, similar to a bruise but just different, more "creeping" but not streaky. Our GP said it was bruising, but it still worries me. As a mom, I want to tear the darned thing off and take a look to make sure everything is okay [I won't of course...lol] - but I get worried about infection.
4. Her foot is still swollen, albeit less so, and a bit irridescent. How long before this goes away? Or will it keep swelling with use [and by use I mean just getting around with her crutches and foot non-weight-bearing].
5. With all of the success stories I hear about with fusion surgeries, why don't they just do that to begin with? Is there a trade-off somewhere in the treatment?
6. From what I understand, she will switch out her post-op slab cast and wrap for a light weight cast at the appointment 17 days post-op, but will still be non-weight-bearing for about 6 weeks. And then she graduates to a removable cast. Swimming has been suggested as a great alternative to keeping things flexible without weight-bearing and I plan to talk to Ortho about it - but does anyone here have experience with using swimming as a rehabilitative route?
7. As far as the ligaments go - I was only involved in a slight conversation in Emerg. about how it can't repair, but the body will lay down scar tissue to compensate for the loss of ligaments. What are peoples' experiences with this, and are there things she can do to make the process go more smoothly? Or is it a c**p shoot as far as how it all turns out?
8. She is a hyper-cautious individual, and while this may benefit her in many ways, because she listens to what the docs are telling here... does she run a risk of being too cautious with the injury. She is 8-9 days post injury, should she be flexing her toes etc?
This is a difficult injury to read up on, especially for a young active girl. Thanks for any and all replies.
My very sports oriented 18 year old daughter suffered a Lisfranc injury - surgery was done within 18 hours through the Emergency - she has three screws [one from her 1st MT to 1st Cuneiform, one from her 2nd MT to 2nd Cuneiform, and I believe one crosswise]. Not completely sure about the direction of the third screw as I was told where they would put the first two before surgery and that they may need to pin the other 3 MT, however I missed the surgeon before she was released from hospital as he was an Emergency call-in Orthopedic Surgeon but as she is considered an adult he did speak to her post-op. So he did tell her about the third screw, and that they did not use any pins. I will know more in a week at her first Ortho appointment [which will be 17 days post-op].
She's a very active student who is getting around okay in the post-op bindings with her crutches. I do have some concerns and questions.
1. She experiences alot of pain when she gets up from a resting position with her foot up, is this due to the fluids/blood rushing into the foot? It tends to ease off once she's up for a bit, but alot of throbbing at first.
2. She's very active in the sense that she has to get around to classes, just how much should she be resting the foot? And when they say put the foot up, must it be above heart level, or is up on a pillow sufficient?
3. With all of the post-op bindings, how would we tell if there were an infection? [She was given a course of IV antibiotics after surgery and prior to leaving the hospital]. I noticed [near her toes] a mark that resembled a strawberry birth mark, similar to a bruise but just different, more "creeping" but not streaky. Our GP said it was bruising, but it still worries me. As a mom, I want to tear the darned thing off and take a look to make sure everything is okay [I won't of course...lol] - but I get worried about infection.
4. Her foot is still swollen, albeit less so, and a bit irridescent. How long before this goes away? Or will it keep swelling with use [and by use I mean just getting around with her crutches and foot non-weight-bearing].
5. With all of the success stories I hear about with fusion surgeries, why don't they just do that to begin with? Is there a trade-off somewhere in the treatment?
6. From what I understand, she will switch out her post-op slab cast and wrap for a light weight cast at the appointment 17 days post-op, but will still be non-weight-bearing for about 6 weeks. And then she graduates to a removable cast. Swimming has been suggested as a great alternative to keeping things flexible without weight-bearing and I plan to talk to Ortho about it - but does anyone here have experience with using swimming as a rehabilitative route?
7. As far as the ligaments go - I was only involved in a slight conversation in Emerg. about how it can't repair, but the body will lay down scar tissue to compensate for the loss of ligaments. What are peoples' experiences with this, and are there things she can do to make the process go more smoothly? Or is it a c**p shoot as far as how it all turns out?
8. She is a hyper-cautious individual, and while this may benefit her in many ways, because she listens to what the docs are telling here... does she run a risk of being too cautious with the injury. She is 8-9 days post injury, should she be flexing her toes etc?
This is a difficult injury to read up on, especially for a young active girl. Thanks for any and all replies.
Loading...
Just as an added curiosity, the ER surgeon who explained the surgery [but not the surgeon who actually did the surgery] said that she would have these screws forever. I've read a lot of talk about when to remove the screws, so could this doctor have been wrong or are there cases where the screws are left in indefinitely or for life? I'll have more information at her Ortho appointment - I just wish more had been explained at the hospital, and our GP isn't very knowledgable on the subject. Thanks.
Loading...
Lisfranc mom-
To answers some of your questions from my own experience...
1. I to had a lot of pain when getting up from a resting position...I assumed it was from the blood going back in to my foot and it did go away after about a month.
2. After I had surgery I was told to keep my foot elevated as much as possible....I was usually only up on it for 20 minutes at a time...and my foot had to be up above my heart...I was off of work for 6 weeks and am just now able to go back for 4 hours a day. This could be different for her though depending on the severity of her injury...I have 2 pins, 9 screws and a plate.
3 & 4. As for infection...her toes are going to be purple liek that for awhile as the swelling increases and decrease...its been almost 8 weeks for me and my foot is still very pink/red in color compared to my other foot. I didn't have my follow-up for 5 weeks post op so as my foot started to get better and the swelling went down the slab cast started to slip down...so I didn't take my wrap off and readjust...then i was able to look at my foot a little bit for infection. The easiest way to monitor for infection is to take her temp every day...she should spike a fever if she had an infection.
5. I hear a foot fusion is very successful as well so I'm not sure why that don't just do that for everyone.
6. I also hear swimming is good for rehab, but she would have to wait until the until the stitches were out and out of the light weight cast...at that point she would get to start bearing weight and probably be going through PT?
8. I was told to wiggles my toes as much as I could to keep the blood flowing and to keep from getting a blood clot.
I was told by my own othro that some of the screws may never come out as well asn some my stay in for over a year.This is something I think that is controversial between different orthos. If they are giving your daughter a lot of pain after all the recovery is completed, it might be something to get another opinion about...or at least that is what I tell myself I will do.
Best of luck to you and your daughter...I feel your concerns for the unknown and her pain!! It will get better though.
To answers some of your questions from my own experience...
1. I to had a lot of pain when getting up from a resting position...I assumed it was from the blood going back in to my foot and it did go away after about a month.
2. After I had surgery I was told to keep my foot elevated as much as possible....I was usually only up on it for 20 minutes at a time...and my foot had to be up above my heart...I was off of work for 6 weeks and am just now able to go back for 4 hours a day. This could be different for her though depending on the severity of her injury...I have 2 pins, 9 screws and a plate.
3 & 4. As for infection...her toes are going to be purple liek that for awhile as the swelling increases and decrease...its been almost 8 weeks for me and my foot is still very pink/red in color compared to my other foot. I didn't have my follow-up for 5 weeks post op so as my foot started to get better and the swelling went down the slab cast started to slip down...so I didn't take my wrap off and readjust...then i was able to look at my foot a little bit for infection. The easiest way to monitor for infection is to take her temp every day...she should spike a fever if she had an infection.
5. I hear a foot fusion is very successful as well so I'm not sure why that don't just do that for everyone.
6. I also hear swimming is good for rehab, but she would have to wait until the until the stitches were out and out of the light weight cast...at that point she would get to start bearing weight and probably be going through PT?
8. I was told to wiggles my toes as much as I could to keep the blood flowing and to keep from getting a blood clot.
I was told by my own othro that some of the screws may never come out as well asn some my stay in for over a year.This is something I think that is controversial between different orthos. If they are giving your daughter a lot of pain after all the recovery is completed, it might be something to get another opinion about...or at least that is what I tell myself I will do.
Best of luck to you and your daughter...I feel your concerns for the unknown and her pain!! It will get better though.
Loading...
Amberjoy, I was non-weight bearing in a cast for 12 weeks with wheelchair and walker, than to a walking cast and crutches for another 8 weeks, than to a custom orthotic shoe with cane which I still use today. I am 4.5 yars post surgery with 7 screws and now have a deformed foot. but i was misdiagnosed with sprain for 7 months too. I know your pain!!! LF injury is the worst foot injury you can have and is life altering. Every situation is different, but with me I can no longer climb stairs, walk normally or without pain, run, jog, hike etc. When you are ready to go back into a shoe you will need a good rocker bottom sole and probably custom orthotics. I have a custom orthotic and have the Drew Blaze shoe that I got at , but there are many good rocker bottom shoes avalable. this one just fits my 4EEEE foot. I wish you well and keep us posted on your progress . I rely on my faith in JC and pain meds to get through every day. Stay positive, Follow your doctors orders to the T, and stay off your foot. It takes time to heal and you only have 2 feet. .
***this post is edited by moderator *** *** private e-mails not allowed **
Please read our Terms of Use
***this post is edited by moderator *** *** private e-mails not allowed **
Please read our Terms of Use
Loading...
Well, I went in for my re-check today. It's been 8 weeks to the day of my surgery and 9 weeks to the day of my injury. The doctor said the bones have healed nicely. I was able to get the 2 pins taken out today, but will remain non weight bearing for another 4 weeks. Then it's back in to be fitted for an orthotic. These 4 weeks won't go fast enough! Then another 10 days before it comes in. I have to say I am really disappointed I can't walk yet and even more so that I won't be able to walk my 2 1/2 year old son door to door trick or treating :-(
Loading...
That is disappointing but he will have other Halloweens so stay strong. I wish you luck--let me know how you're doing okay?
Loading...
Hi All,
So i'm not sure if i have a lisfranc injury or not but I'm really nervous that I might have one. So here is my story...I spent the month of August on crutches (non-weightbearing) to heal a stress fracture in my left hip (femur neck). Somehow, I managed to suffer a injury to my left foot about 4 weeks into non-weightbearing. I was at my father's house and I was sleeping on my back so I wouldn't put pressure on my hip. The sheets/bedding were tucked into the bed extremely tight and, since I was on my back, I fell asleep with my foot held in a dorsiflexed position (foot bent back towards my body) by the sheets. Now i'm not sure exactly what I did in my sleep (possibly hyperflexed the foot back) but I awoke in the middle of the night with a intense pain (almost like a charlie horse) in the top of my foot. I thought that it was just a cramp so I tried to massage the foot causing a burning type of pain to spread throughout the top of my foot. I took tylenol. This intense pain lasted for about 5-10 minutes or so before it started to ease. I went back to bed. The next day I noticed a sharp pain in the top of my foot if i bent the foot up. Later on that day, I put my sneakers on and felt that my shoe seemed tighter on the left foot. I took my shoe off and saw that my foot was slightly swollen. There was no bruising though. The sharp pain when I ever I held my foot up continued for the final 2 weeks of my non-weightbearing. The swelling went away as soon as I started using the foot again but I felt sharp pains on top of my foot whenever I walked on it. I have been walking for 4 weeks now and still feel a sharp pain in my mid-foot when I push off the foot. It is probably about a 2 out of 10 in terms of intensity and isn't as bad as when I first started walking. There doesn't appear to be swelling or bruising and isn't tender to touch. My ankle aches. It doesn't bother me as much in high heels, when I am my running sneakers, or my vans/skater sneakers. I had it checked out by a doctor a week ago. She sent me for x-rays of the foot (non-weightbearing) to rule out a stress fracture. They came back normal. I was pretty upset still because I don't think i would be experiencing pain after a month and half if it were something minor like strained ligaments so she sent me for an MRI. I went last night but haven't gotten the results yet. I also went to a podiatrist last week and he said there is no way i could have a lisfranc sprain because my foot would be extremely swollen. I'm not entirely convinced. Is it possible that my symptoms could be a lisfranc sprain? I know i'll find out on Monday but i'm really anxious.
So i'm not sure if i have a lisfranc injury or not but I'm really nervous that I might have one. So here is my story...I spent the month of August on crutches (non-weightbearing) to heal a stress fracture in my left hip (femur neck). Somehow, I managed to suffer a injury to my left foot about 4 weeks into non-weightbearing. I was at my father's house and I was sleeping on my back so I wouldn't put pressure on my hip. The sheets/bedding were tucked into the bed extremely tight and, since I was on my back, I fell asleep with my foot held in a dorsiflexed position (foot bent back towards my body) by the sheets. Now i'm not sure exactly what I did in my sleep (possibly hyperflexed the foot back) but I awoke in the middle of the night with a intense pain (almost like a charlie horse) in the top of my foot. I thought that it was just a cramp so I tried to massage the foot causing a burning type of pain to spread throughout the top of my foot. I took tylenol. This intense pain lasted for about 5-10 minutes or so before it started to ease. I went back to bed. The next day I noticed a sharp pain in the top of my foot if i bent the foot up. Later on that day, I put my sneakers on and felt that my shoe seemed tighter on the left foot. I took my shoe off and saw that my foot was slightly swollen. There was no bruising though. The sharp pain when I ever I held my foot up continued for the final 2 weeks of my non-weightbearing. The swelling went away as soon as I started using the foot again but I felt sharp pains on top of my foot whenever I walked on it. I have been walking for 4 weeks now and still feel a sharp pain in my mid-foot when I push off the foot. It is probably about a 2 out of 10 in terms of intensity and isn't as bad as when I first started walking. There doesn't appear to be swelling or bruising and isn't tender to touch. My ankle aches. It doesn't bother me as much in high heels, when I am my running sneakers, or my vans/skater sneakers. I had it checked out by a doctor a week ago. She sent me for x-rays of the foot (non-weightbearing) to rule out a stress fracture. They came back normal. I was pretty upset still because I don't think i would be experiencing pain after a month and half if it were something minor like strained ligaments so she sent me for an MRI. I went last night but haven't gotten the results yet. I also went to a podiatrist last week and he said there is no way i could have a lisfranc sprain because my foot would be extremely swollen. I'm not entirely convinced. Is it possible that my symptoms could be a lisfranc sprain? I know i'll find out on Monday but i'm really anxious.
Loading...
To cgp83
From what you have written, I think that it is extremely unlikely that you have a lisfranc injury. Don't worry too much. Good luck.
From what you have written, I think that it is extremely unlikely that you have a lisfranc injury. Don't worry too much. Good luck.
Loading...
Thanks Gymnasticsnz,
That is what I have been told by my doctors, physical therapist, and family. I just came back from a serious hip injury & am currently in PT to learn to live with a labral tear in my hip. I'm making great progress with the hip so it would be devastating if I am unable to get back to my active lifestyle because I managed to injur my foot while on crutches. Not to mention i'm not sure if I can handle crutches & NWB again. I guess I'll finally know what is going on with my foot tomorrow.
That is what I have been told by my doctors, physical therapist, and family. I just came back from a serious hip injury & am currently in PT to learn to live with a labral tear in my hip. I'm making great progress with the hip so it would be devastating if I am unable to get back to my active lifestyle because I managed to injur my foot while on crutches. Not to mention i'm not sure if I can handle crutches & NWB again. I guess I'll finally know what is going on with my foot tomorrow.
Loading...
Newbie story alert!
Short version - 22 Sept 09 horse-riding crush injury, operated on 23 Sept - 6 screws, 2 external pins, lis franc ligament reconstructed, compartment sydrome, fasciotomies which were closed 26 Sept, discharged 29 Sept. Stitches removed 15 Sept. No pain since discharge apart from when it was infected but 1wk course of strong antibiotics cleared it, non weight bearing, currently in back-slab cast until next review on 29 Sept - before cast was put on had good level of mobility in the ankle and toes and was massaging the calf to encourage drainage. Pins due to come out 5 Nov, then into a cast - I wasn't clear whether full cast or walking cast, but I think it's full cast for 6 weeks to be on track to be weight bearing in walking cast at 12 weeks and will be referred for intensive physio which would go along with most of the experiences here. Bought a 2nd hand wheelchair which is invaluable and has made a huge difference to my ability to get out of the house without tiring myself out too much. I have amazing housemates who are looking after me really well and helping to keep my spirits up.
Photos and x-rays at
Thank you to everyone who's shared their story and progress on this site - although there is a really wide variety of outcomes, it has helped to know that there is at least hope of a reasonable recovery eventually. I am a feisty, determined gal and I am going to return to my previous activity level as soon as I can.
Long and boring version - my horse fell sideways while I was riding, and her body crushed my foot at 13.45 on 22 September 2009. I felt the foot swell instantly inside my boot and knew it was bad. The ride to hospital was the most excruciating 30 minutes of my life. I was taken almost straight in and x-rayed, then told that I had a rare Lisfranc injury and was going to be referred to one of the specialist centres here in Northern Ireland. I had my iPhone with me and made the mistake of googling Lisfranc injury - scared myself silly but was reassured by the fact it was being taken so seriously and was grateful for the codeine! I was transferred to the Royal Victoria Hospital by 7.30pm and given painkillers overnight. I hadn't eaten anything since 6pm the day before so my blood pressure went through the floor at times and I was turned into a pin cushion because they couldn't get a venflon in anywhere they tried (5 places) so a doctor came to do it at 4am.
The surgeon came round at 9am and suspected compartment syndrome so bumped me to second on the list (I had to have a chest x-ray first due to crappy asthma). Because my lungs weren't so good I was operated on using a lower leg nerve block, spinal anaesthetic and sedation at 11am - there were 5 surgeons and it was very surreal drifting between sleep and awareness, I wanted to see what they were doing but only made myself feel confused so asked for more sedation at that point. I was taken to recovery at 1pm and had to wait there until 8.30pm until a bed became free on the ward. Thankfully they made an exception and allowed my best friend to visit me in recovery from 7pm and stay with me until 10.30pm (well outside visiting hours), as I have no family over here.
I ended up with 3 incisions in the foot, each approximately 10cm long - the one on my arch was closed in this operation but two on the top of the foot were left open to allow the pressure to dissipate by letting fluid drain and avoid any damage from compartment syndrome. This was unpleasant but necessary. There are 6 screws and 2 temporary external pins in the foot, and they had to repair the ligaments too. I had a morphine pump for pain relief along with codeine, i/v paracetamol and i/v antibiotics (amoxycillin). Unfortunately when the nerve block wore off at 2am after I'd slept for a little while and not needed much morphine because of the nerve block NOTHING worked until I'd had an hour's worth of 1ml morphine every 5 minutes and it was absolute agony. I would never, ever have a nerve block again as there is no guarantee when it will suddenly lose effectiveness.
On 24 September a surgeon came round and told me that I had done really serious damage to the foot and the prognosis was poor - it would never be a normal foot again. 15 minutes after he had dropped this bombshell the physioterrorists came round and got me up - I hadn't used the morphine pump for 90 minutes as there was no pain unless I moved and I had been keeping it pretty still. The blood rush to the foot was more agony, I burst into tears and begged them to come back later so I could have pain relief, which they agreed to do. I rang my friend in tears and we both cried. Physios came back later and I did a little bit on a 'walker' and then a few metres on crutches - big positive turn!
I muddled along getting gradually more mobile, and on 26 Sept had a futher operation (this time under GA) to close the fasciotomy incisions. On 27 Sept I had the morphine pump removed in the morning but unfortunately fell while trying to get to the toilet that evening and hurt the foot but thankfully didn't do any damage. This knocked my confidence but I recovered it and was discharged on 29 Sept.
Dressings were changed every 3-4 days, infection discovered after 1 week and treated successfully with co-amoxiclav. 2.5 weeks post-op returned to fracture clinic for stitches to be removed, Dr pleased with progress and lack of pain. Back to clinic on 29 Oct for checkup, pins to come out 5 Nov.
I am mostly pretty optimistic - watch this space!
Short version - 22 Sept 09 horse-riding crush injury, operated on 23 Sept - 6 screws, 2 external pins, lis franc ligament reconstructed, compartment sydrome, fasciotomies which were closed 26 Sept, discharged 29 Sept. Stitches removed 15 Sept. No pain since discharge apart from when it was infected but 1wk course of strong antibiotics cleared it, non weight bearing, currently in back-slab cast until next review on 29 Sept - before cast was put on had good level of mobility in the ankle and toes and was massaging the calf to encourage drainage. Pins due to come out 5 Nov, then into a cast - I wasn't clear whether full cast or walking cast, but I think it's full cast for 6 weeks to be on track to be weight bearing in walking cast at 12 weeks and will be referred for intensive physio which would go along with most of the experiences here. Bought a 2nd hand wheelchair which is invaluable and has made a huge difference to my ability to get out of the house without tiring myself out too much. I have amazing housemates who are looking after me really well and helping to keep my spirits up.
Photos and x-rays at
Thank you to everyone who's shared their story and progress on this site - although there is a really wide variety of outcomes, it has helped to know that there is at least hope of a reasonable recovery eventually. I am a feisty, determined gal and I am going to return to my previous activity level as soon as I can.
Long and boring version - my horse fell sideways while I was riding, and her body crushed my foot at 13.45 on 22 September 2009. I felt the foot swell instantly inside my boot and knew it was bad. The ride to hospital was the most excruciating 30 minutes of my life. I was taken almost straight in and x-rayed, then told that I had a rare Lisfranc injury and was going to be referred to one of the specialist centres here in Northern Ireland. I had my iPhone with me and made the mistake of googling Lisfranc injury - scared myself silly but was reassured by the fact it was being taken so seriously and was grateful for the codeine! I was transferred to the Royal Victoria Hospital by 7.30pm and given painkillers overnight. I hadn't eaten anything since 6pm the day before so my blood pressure went through the floor at times and I was turned into a pin cushion because they couldn't get a venflon in anywhere they tried (5 places) so a doctor came to do it at 4am.
The surgeon came round at 9am and suspected compartment syndrome so bumped me to second on the list (I had to have a chest x-ray first due to crappy asthma). Because my lungs weren't so good I was operated on using a lower leg nerve block, spinal anaesthetic and sedation at 11am - there were 5 surgeons and it was very surreal drifting between sleep and awareness, I wanted to see what they were doing but only made myself feel confused so asked for more sedation at that point. I was taken to recovery at 1pm and had to wait there until 8.30pm until a bed became free on the ward. Thankfully they made an exception and allowed my best friend to visit me in recovery from 7pm and stay with me until 10.30pm (well outside visiting hours), as I have no family over here.
I ended up with 3 incisions in the foot, each approximately 10cm long - the one on my arch was closed in this operation but two on the top of the foot were left open to allow the pressure to dissipate by letting fluid drain and avoid any damage from compartment syndrome. This was unpleasant but necessary. There are 6 screws and 2 temporary external pins in the foot, and they had to repair the ligaments too. I had a morphine pump for pain relief along with codeine, i/v paracetamol and i/v antibiotics (amoxycillin). Unfortunately when the nerve block wore off at 2am after I'd slept for a little while and not needed much morphine because of the nerve block NOTHING worked until I'd had an hour's worth of 1ml morphine every 5 minutes and it was absolute agony. I would never, ever have a nerve block again as there is no guarantee when it will suddenly lose effectiveness.
On 24 September a surgeon came round and told me that I had done really serious damage to the foot and the prognosis was poor - it would never be a normal foot again. 15 minutes after he had dropped this bombshell the physioterrorists came round and got me up - I hadn't used the morphine pump for 90 minutes as there was no pain unless I moved and I had been keeping it pretty still. The blood rush to the foot was more agony, I burst into tears and begged them to come back later so I could have pain relief, which they agreed to do. I rang my friend in tears and we both cried. Physios came back later and I did a little bit on a 'walker' and then a few metres on crutches - big positive turn!
I muddled along getting gradually more mobile, and on 26 Sept had a futher operation (this time under GA) to close the fasciotomy incisions. On 27 Sept I had the morphine pump removed in the morning but unfortunately fell while trying to get to the toilet that evening and hurt the foot but thankfully didn't do any damage. This knocked my confidence but I recovered it and was discharged on 29 Sept.
Dressings were changed every 3-4 days, infection discovered after 1 week and treated successfully with co-amoxiclav. 2.5 weeks post-op returned to fracture clinic for stitches to be removed, Dr pleased with progress and lack of pain. Back to clinic on 29 Oct for checkup, pins to come out 5 Nov.
I am mostly pretty optimistic - watch this space!
Loading...
Optimisim is the BEST attitude to have going into this sort of thing so I'm glad to hear that you've got a good attitude about it. Let me know how you're doing, okay?
Loading...
Hi and thank you hnfg! I have now registered - the long guest post above is me.
My optimism is not as strong as it was, but this has coincided with having 10 days with my parents which is always somewhat traumatic even when I am mobile so I am pretty tired - their house is noisy and I found it hard to settle. I started off unable to get my head around the steps into the house and my poor dad had to half lift me up but I have to say by the end of the 10 days my confidence in using the crutches has soared, especially for steps and uneven ground.
I took the temporary cast off on 23 Oct as the airline I flew back with wouldn't let me fly with a plaster cast without a doctor's note, the local doc at my folks' wouldn't say I was fit to fly without having my notes, my own doc wouldn't say I was OK to fly without seeing me and I got very stressed about potentially being stranded. I know that it was potentially a stupid thing to do but I figured that since the docs weren't worried about immobilising it for the first 3.5 weeks, the physio had said the more movement the better, and the temporary cast was actually holding it at neutral rather than the 90 degrees the doc had wanted in order to prevent tendon contraction, on balance it was OK as it would give me the opportunity to massage and wiggle to my heart's content as well as bringing the foot up to 90 degrees as much as possible. It had been itching very badly anyway, and my toes were going purple as soon as I lowered the foot, which they hadn't been for the 3.5weeks where I had just a bandage - presumably because I was unable to move my ankle and contract/massage my calf to promote circulation. The leg and foot are now much more comfortable, but I am not looking forward to the roasting I am likely to get upon my return to the hospital. I am getting the dressing changed in the morning at the local surgery and can't wait to see what it looks like now the stitches are out and the skin should have healed!
I am feeling low at times because of being such a burden on my friends - I don't have many over here yet, so the two that I live with are shouldering more than their fair share and I feel guilty about that. We have also gone to winter time so it is getting dark at 5pm and the lack of daylight combined with nil exercise is giving me the blues already - my cheery, chirpy self is hard work right now and my sense of humour is failing. I have bought a 'daylight' lamp to try and combat this, and am going to try some natural anti-depressants too as I really don't want to wait for this to get any worse. I am researching battery powered heated insoles for my boots and am going to ask for some for Christmas, to try to ward off any pain from the cold, damp weather that we get here for half the year.
I just noticed that my facebook link above was deleted - the album of photos (some gory) is at and i should have some new ones in
about 12 hours.
***edited by moderator*** web addresses not allowed
My optimism is not as strong as it was, but this has coincided with having 10 days with my parents which is always somewhat traumatic even when I am mobile so I am pretty tired - their house is noisy and I found it hard to settle. I started off unable to get my head around the steps into the house and my poor dad had to half lift me up but I have to say by the end of the 10 days my confidence in using the crutches has soared, especially for steps and uneven ground.
I took the temporary cast off on 23 Oct as the airline I flew back with wouldn't let me fly with a plaster cast without a doctor's note, the local doc at my folks' wouldn't say I was fit to fly without having my notes, my own doc wouldn't say I was OK to fly without seeing me and I got very stressed about potentially being stranded. I know that it was potentially a stupid thing to do but I figured that since the docs weren't worried about immobilising it for the first 3.5 weeks, the physio had said the more movement the better, and the temporary cast was actually holding it at neutral rather than the 90 degrees the doc had wanted in order to prevent tendon contraction, on balance it was OK as it would give me the opportunity to massage and wiggle to my heart's content as well as bringing the foot up to 90 degrees as much as possible. It had been itching very badly anyway, and my toes were going purple as soon as I lowered the foot, which they hadn't been for the 3.5weeks where I had just a bandage - presumably because I was unable to move my ankle and contract/massage my calf to promote circulation. The leg and foot are now much more comfortable, but I am not looking forward to the roasting I am likely to get upon my return to the hospital. I am getting the dressing changed in the morning at the local surgery and can't wait to see what it looks like now the stitches are out and the skin should have healed!
I am feeling low at times because of being such a burden on my friends - I don't have many over here yet, so the two that I live with are shouldering more than their fair share and I feel guilty about that. We have also gone to winter time so it is getting dark at 5pm and the lack of daylight combined with nil exercise is giving me the blues already - my cheery, chirpy self is hard work right now and my sense of humour is failing. I have bought a 'daylight' lamp to try and combat this, and am going to try some natural anti-depressants too as I really don't want to wait for this to get any worse. I am researching battery powered heated insoles for my boots and am going to ask for some for Christmas, to try to ward off any pain from the cold, damp weather that we get here for half the year.
I just noticed that my facebook link above was deleted - the album of photos (some gory) is at and i should have some new ones in
about 12 hours.
***edited by moderator*** web addresses not allowed
Loading...