European diabetics have a "new" form of long-lasting insulin, Abasria, which is a "biosimilar" product that is chemically identical to the American product Lantus. Approving this new insulin will probably drive down prices for European health agencies that buy the product in bulk for their entire countries, but will have no effect on insulin prices for most Europeans - who get their insulin under nationally managed health insurance plans - or for most diabetics in the USA--where only Lantus is approved.
But using long-lasting insulins correctly can make a huge difference for children and adults who have diabetes. Here's what diabetics and the parents of American children need to know about long-lasting insulin, starting with the basics.
Long-lasting insulins are given in larger doses, and the dosage makes the difference.
Most diabetics who have to use insulin are told that Humolog R and Novolog and similar products are "fast acting" insulins to be taken in smaller doses just before meals, and Humulin N and Lantus are "slow acting" or basal insulins that are taken in larger doses once or maybe twice a day to cover the slow upward creep of blood sugar levels during sleep or after strenuous exercise. (As an aside, strenuous exercise, despite what diabetics are told, raises blood sugar levels, while slow exercise lowers them.)
A diabetic might be told to inject 10 units of Novolog 20 minutes before every meal and 50 units of Lantus twice a day in the morning and in the evening. But the fact is, "fast" insulin can last 24 hours, if you take enough, and "slow" insulin can cover the increase in blood sugars after your meals if you follow your prescribed diet.
Any kind of insulin you take in a dose of more than 7 units (as they are measured in the US) becomes a "long lasting" insulin.
The fact is, any insulin you take in a large dose (large being what is large for you) becomes long-acting. Any dose of insulin greater than 7 units is incompletely absorbed into the bloodstream.
We aren't going to tell you not to follow your doctor's orders regarding the insulin you use. But we do suggest that if you are having trouble coming up with $220 a vial for Lantus, or if your local pharmacy doesn't stock the newly approved Abasria, ask if there is not some way to change the dosage of less expensive insulins for you or your child to keep your blood sugar levels in check.
See Also: FDA Approved: Inhaled Insulin For Diabetes
And we're certainly not going to tell you to take less insulin. If you are currently taking 30 units of Novolog a day and 100 units of Lantus a day, then dropping down to just 30 units a day isn't going to keep you blood sugar levels in check. You almost certainly need the same number of units of insulin every day, until you make changes in diet and exercise or other medications. But you may be able to keep your sugars regulated with insulin that does not cost as much.
Seven Tips For Using Insulin Effectively
- Don't inject insulin into the exact location every day. The skin and tissues underlying it can develop an "allergy" to insulin that creates inflammation and thickening of the skin that reduces the blood sugar control you get from your shot. Inject in different locations and don't inject into the same site more often than once every 2 weeks.

- Don't inject more than 7 to 10 units of insulin at a time. If you have to take 20, 30, 40 or more units to control your blood sugars, inject 7 to 10 units in one site, remove the needle, inject another 7 to 10 units in another location, remove the needle, inject a third 7 to 10 units into a third location, and so on. This reduces autoimmune reactions to insulin and allergies to chemicals acting to the insulin and gets more insulin into your bloodstream, where it is needed.
- Let your skin meet the needle, don't jab the needle into your skin. Hold the syringe with one hand while you depress your skin with the other. Release your skin so it springs into the needle, and then press on the plunger to release insulin. This keeps the shot from hurting, and reduces the risk of hitting a vein and getting too much insulin into your bloodstream too fast.
- Follow your diabetes diet so you don't have to use as much insulin. Small inputs result in small errors. You are less likely to have to deal with hypoglycemia (low blood sugars) or hyperglycemia (high blood sugars) if you eat less and use less insulin. And since insulin also regulates how your fat cells store fat, locking it inside them, or release fat for your muscles to burn, the less insulin you have to take, the easier it will be for you to maintain your weight or lose weight.
- When you use the "cheap stuff" you buy at Costco or Walmart without a prescription because your prescription insulin has run out and your insurance company will not let you have more, be sure to measure your blood sugar levels several times a day. Different brands of insulin contain different chemicals in trace amounts, and lower blood sugars at slightly different rates.
- The secret to successful use of insulin testing your blood sugar levels several times a day. Generic, low-cost test strips really aren't as accurate as prescription brands, but if you compare the numbers your get at home with the numbers you are given at your doctor's office you can tell whether your strips run low (as they usually do, since there would be greater legal liability to the company makes the strips for undetected hypoglycemia) or low. Ideally, every time you use insulin, you should test your blood sugar levels 2 or 3 hours later, and adjust insulin or food intake accordingly.
See Also: Insulin: The Only Medication For Diabetes That Always Work
- Insulin is the only medication for diabetes that always works--if you use enough. But if you start taking other medications, be aware that you need to do all your prescribed testing to make sure your blood glucose levels don't run too low.
- Tucker ME. EMA Advisory Panel Recommends First Biosimilar Insulin. International Approvals--Medscape Medical News. 27 June 2014.
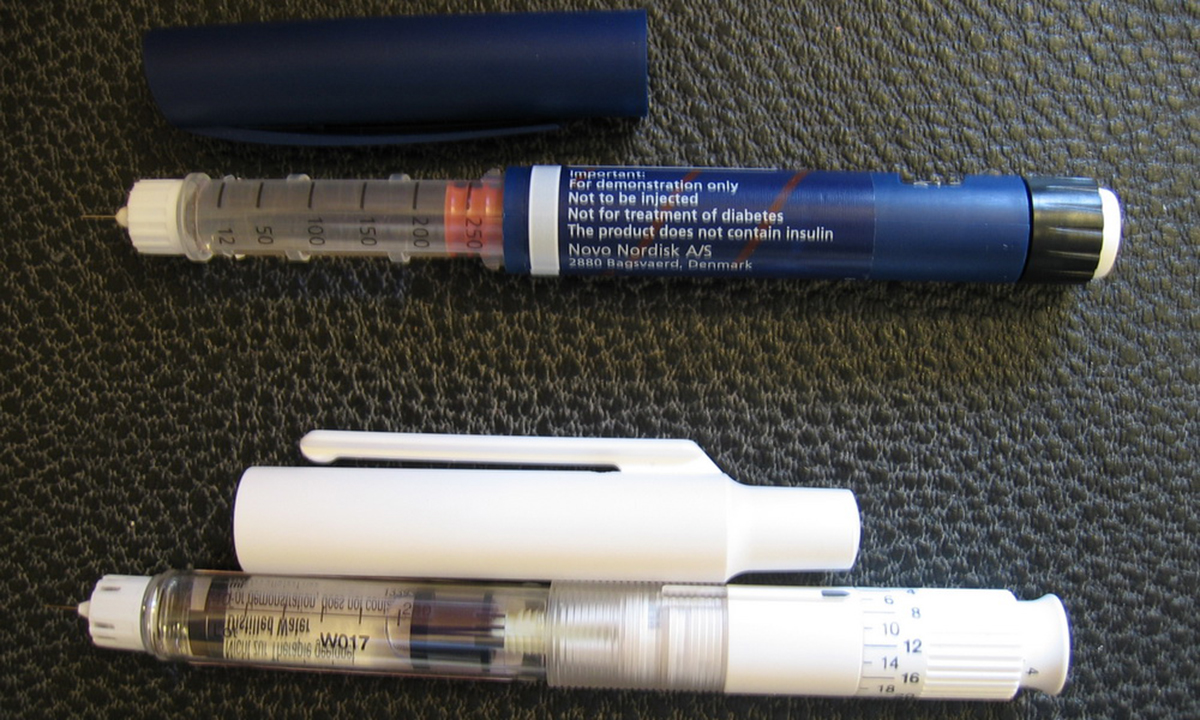
- Photo courtesy of PerPlex by Wikimedia Commons : en.wikipedia.org/wiki/Insulin_pen#mediaviewer/File:Insulin_pen.JPG
- Photo courtesy of Tony Alter by Flickr : www.flickr.com/photos/78428166@N00/8760624945/


Your thoughts on this