Table of Contents
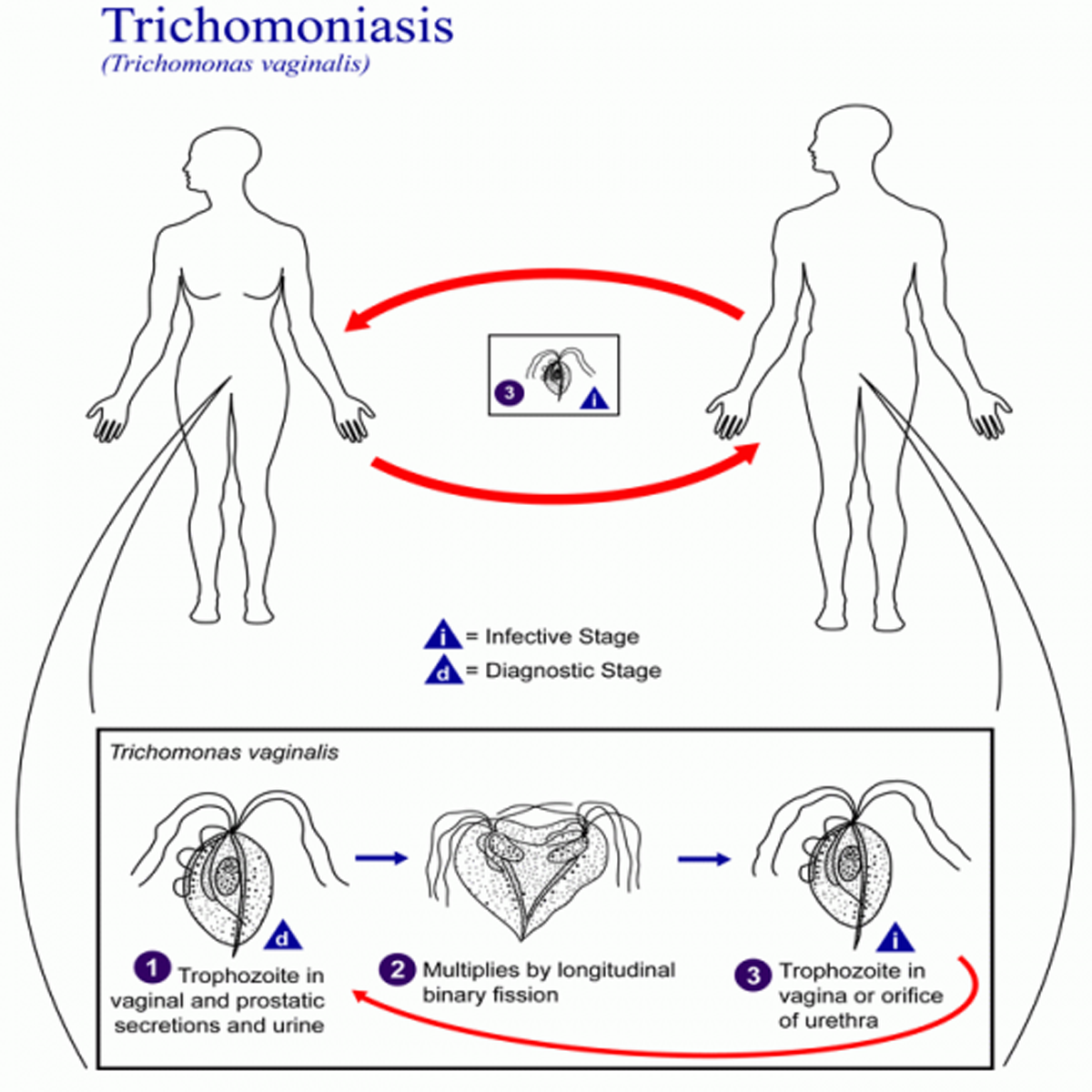
The problem is that trichomoniasis, like many other STDs, often occurs without any symptoms. Men almost never have symptoms, while women can have symptoms and they usually appear within four to 20 days after the exposure. Trichomoniasis is primarily an infection of the uro-genital tract. The urethra is the most common site of infection in man, while the vagina is the most common site of infection in women.
Women
- discharge from your vagina that is green or yellow.
- discharge from your vagina that smells like fish, especially after sex.
- itching, red, or sore vagina.
- blood spotting in vaginal discharge
- swelling in the groin
- swollen and irritated vagina and cervix
- urinating more than usual
- worsening symptoms when menstruating
- pain when you urinate.
- pain when you have vaginal intercourse.
- lower abdominal pain in rare cases
Men
- infection of the urethra or prostate gland, which is involved in semen production
- a small amount of clear discharge from your penis.
- burning or itching around the opening of your penis.
- burning feeling in your penis after having sex.
- pain when you urinate.
- tingling inside the penis
It is very important to know that person may not have symptoms but still have the infection.
Risk factors for developing trichomoniasis
Risk factors for T vaginalis include the following:
- Infection with other STDs, especially gonorrhea
- Four or more lifetime sex partners
- Sexual contact with an infected partner
- Not using barrier contraception
Complications of trichomoniasis
It is proven that untreated trichomoniasis can be linked to several other conditions of which some are very serious. The prolonged infection may cause changes in the tissue of the cervical surface. It can also lead to an increased risk for HIV infection. Infected pregnant women are at risk for premature birth, low birth weight, and infection or rupture of the placenta. Inflammation of the prostate and bladder are associated with trichomoniasis in men.
Diagnosis of trichomoniasis
Diagnosis can be made by:
Pelvic examination
A pelvic examination reveals red blotches on the vaginal wall or cervix. It may also reveal a distinctive, inflamed cervix. During the pelvic exam, doctor is usually able to see small red sores inside the vagina or on the cervix. For both men and women, a health care provider must perform a physical examination and laboratory test to diagnose trichomoniasis. The parasite is harder to detect in men than in women.
Examination under a microscope
A wet prep or microscopic examination of discharge demonstrates rapidly moving trichomonads in the vaginal secretions. Sensitivity is poor, 40-60%.
Pap smears
A pap smear may also detect the presence of the organism. Sensitivity is similar to that of wet mount, 60%.
Culture Tests
A culture of the organism or an antibody test may be done, especially in men, as relatively few of the parasites are found in discharges from the penis
OSOM Trichomonas Rapid Test
This is a very modern because it uses color immune-chromatographic “dipstick” technology with monoclonal antibodies and results are read within 10 minutes. The sensitivity is 83.3% and specificity is 98.8%.
BD Affirm VPIII Microbial Identification Test
This test uses nucleic acid hybridization technology. The great thing about this test is that it has sensitivity of between 90 and 100%.
In men, the disease can be hard to diagnose without special culture techniques, but men are treated presumptively if infection is diagnosed in female sexual partners.
Polymerase chain reaction- PCR
PCR is a very good, efficient and modern diagnostic tool based on DNA amplification and detection using known primers to specific genes. It also has good sensitivity ( 97%), and specificity (98%). In males, performing PCR on urine sediment rather than urethral swabs improves detection rates.
- www.cdc.gov
- www.emedicine.com
- www.nlm.nih.gov
- en.wikipedia.org/wiki/Trichomoniasis
- Photo courtesy of /Alexander J. da Silva, PhD/Melanie Moser by Wikimedia Commons : commons.wikimedia.org/wiki/File:Trichomoniasis_01.png

