I Too have the exact same problem. vaginal pasty white discharge, not a yeast infection, dizziness, abdominal pain, and I also have flushing.
How old are all of you?
Any possibility of having low estrogen levels?
How old are all of you?
Any possibility of having low estrogen levels?
Loading...
im 14, and i had the same exact problem. except i figured out that if you "scoop it out" until there's none left, and do that when ever you get the wet toilet discharge, it goes away. at least for me it did. you have to be really comfortable with your body though. just every time you get some out, rinse your hands with water and do it again.
Loading...
Hello ladies. I have expereinced the same thing. Sounds like BV (Bacterial Vaginosis). By chance is anyone using Metrogel. I found when my GYN perscribs Metrogel, I get the same white-toilet paper discharge. Its normal and will usually go away a few days after use.
Loading...
i also have this but im 17 and i have the same thing but i also dont know what it is but i also was ichy and its off and on at times it goes away and then it comes back,
Loading...
I also am experiencing this and never in the last 20 some years that I have been sexual active has this happened. I am also freakin out because there is no symptoms of an yeast infection either. I have also, as some else stated, had problems in the past few month with bloating and digesting. I thought that I was having constipation problems so i ordered a herbal remedy called naturally young intra cleanse. Part of the daily routine is taking these pills twice a day with a multi-vitamin and Achia Berry, although it is working well. I am wondering if this is messing with my natural chemical balance. Or do I have a disease? I wish someone would come up with something other than a yeast infection, because thats not what this is. Iam glad to know I am not alone. This is bizarre and scary.
Loading...
I have had this problem off and on for about a year. No STD's, not pregnant. I was just treated for BV (no symptoms of it, just found out at a routine exam) with Clindesse, and the clumpiness returned after the treatment. I'm thinking it's a hormonal thing. I've told my doctor numerous times and she doesn't seem to be very concerned :?
Loading...
So strange, I've had this same white, clumpy discharge closer to my period. I've been to the doctor and they say everything is "normal".....WEIRD
Loading...
i have the same problem that the other posters have said, no irritation, just the white clumpy discharge. I've had it for a couple of weeks now..it doesnt cause any major problems but sometimes its worse than others..i'd really like to know what it is though.
Loading...
I have had the same issues as all above...white, clumpy, curd-like, "scoop-able", discharge, not yeast or BV, gets worse prior to menstruation. I was also having lots of irritation and dryness that led to discomfort and pain during sex. I even brought up my issues to my GYN and she changed my oral contraceptives and wrote it off as nothing. Which was frustrating since the problem persisted. I even stopped the oral contraceptives to see if it was hormonally related...and it didn't go away. I did look up cytolytic vaginosis and found some helpful support:
http://www.virginia.edu/studenthealth/Cytolytic%20Vaginosis.pdf
I tried the vaginal baking soda suppository, 2 times a week for 2 weeks and have had some alleviation of symptoms, especially the dryness and irritation. I ordered size 00 empty gelatin capsules and filled them with baking soda. A few words of warning for this treatment: baking soda stings cuts, so if you have any small cuts on your labia or surrounding area, it really burns...avoid this treatment when you have cuts! Also, it also made me very wet, like felt like I pee'd in my pants...most likely due to the vaginal membranes reacting to the alkalinity. I recommend wearing a maxi-pad to keep you dry and prevent an embarrassing white mark on your pants when the baking soda dries!
I imaging a baking soda douche would provide the same relief, but I found the gelatin capsules to be easier and more discreet. An additional "symptom" that seems to be linked to this issue was plaguing my husband. After unprotected sex, he would get small, red dots on the head of his penis that would be irritated and then get dry and go away. No risk of STDs, and this tended to correlate with my "episodes" and condoms prevented it. I don't know if the baking soda treatment of myself helps this issue since we're using condoms for contraception...perhaps when it's time for babies we'll find out...
Sorry for the lengthy post, I just hope this helps someone because I understand the frustration!
http://www.virginia.edu/studenthealth/Cytolytic%20Vaginosis.pdf
I tried the vaginal baking soda suppository, 2 times a week for 2 weeks and have had some alleviation of symptoms, especially the dryness and irritation. I ordered size 00 empty gelatin capsules and filled them with baking soda. A few words of warning for this treatment: baking soda stings cuts, so if you have any small cuts on your labia or surrounding area, it really burns...avoid this treatment when you have cuts! Also, it also made me very wet, like felt like I pee'd in my pants...most likely due to the vaginal membranes reacting to the alkalinity. I recommend wearing a maxi-pad to keep you dry and prevent an embarrassing white mark on your pants when the baking soda dries!
I imaging a baking soda douche would provide the same relief, but I found the gelatin capsules to be easier and more discreet. An additional "symptom" that seems to be linked to this issue was plaguing my husband. After unprotected sex, he would get small, red dots on the head of his penis that would be irritated and then get dry and go away. No risk of STDs, and this tended to correlate with my "episodes" and condoms prevented it. I don't know if the baking soda treatment of myself helps this issue since we're using condoms for contraception...perhaps when it's time for babies we'll find out...
Sorry for the lengthy post, I just hope this helps someone because I understand the frustration!
Loading...
I too am having this issue...I've been trying to clean it out in the tub....comes out but looks god aweful! I'm going to my Dr. it reminds me of toilet paper (and I know I don't "shove" TP in there) but it also reminds me of dead skin. I live in an aweful town where the Dr's really don't know what the hell they're talking about when it comes to ANYTHING! But I'll give it a shot, you never know...if I get any answeres I'll let you ladies know. :$
Loading...
I know this is an old thread, but I'm resurrecting it for a reason...
I was having the exact same symptoms as everyone here. It went on for months. Actually, it's still happening. At first I thought I had BV or a yeast infection, but there was no tell-tale odor or anything of the sort. Two rounds of antibiotics did nothing. So when I found this thread, it was incredibly comforting because it was oddly nice to know I wasn't the only one confused by this. Finally, this month it was the worst ever so I went back to the doctor... which is what brings me here...
I know what this is.
For months I was dealing with the discharge. Like you all said - exactly like wet toilet paper and odorless. Sure, it was annoying as heck, but that's all it was. Discharge. (Which is also why I got treated for BV twice... doc and I both thought it was just an infection.) After a while I noticed that for a few days each month I was getting pretty bloated, and as someone mentioned here, almost as if my digestive system "shuts down" in a way. Then, the bloating... but almost like swelling?... kept getting worse and worse. After a few months of it, each bloating "session" would feel as if I gained 50lbs overnight. One of the biggest clues was that the bloating was always the worst right around the time I should be ovulating. Finally, this month, I ended up face down on my desk in pain trying to explain to my boss that I needed to go to the doctor because this is just not right. My back was on fire. It felt like I did too many situps - with my uterus. My breasts were so swollen that the lightest touch to my nipple would practically put me in tears. This had NEVER happened before, but looking back at the progression of this over the months, it probably shouldn't have been a surprise to me. I guess hindsight is 20/20, ya know?
So I now have a diagnosis - Endometriosis.
I didn't find my treatment options all that desirable. Apparently I can go on birth control so I only have a period 3x per year, but over the years I've become very anti-synthetic drugs. That, and the side effects for the pills included things like heart attack and stroke... I don't know, it just put me off. Also, I could have surgery to remove the tissue, but from what I've been reading, the tissue tends to grow back which would mean multiple surgeries. Hmm, so far, not a fan.
So, I've been digging into a lot of research on this and found that much like fibroids, fibrocystic breast disease, ovarian cysts, ovarian cancer and breast cancer, endometriosis seems to go hand in hand with very high levels of estrogen. Another hindsight I suppose since high estrogen conditions (like those mentioned above) seem to run in my family.
I've decided to treat this for myself I'm going to look into natural ways to lower my estrogen levels. I figure, if need be, the birth control pills are always there as a fallback plan. But, I'm still learning about this myself... if you'd like to get more information, I suggest googling things like "estrogen dominance" and "+endometriosis +estrogen". And the reason I tell you this is because, it might be worth looking into getting your estrogen levels under control before this 'kind of annoying' condition turns into 'face down on your desk in throbbing pain' like mine did. I really wouldn't wish that kind of pain on anyone.
I hope I haven't scared anyone. It's not a death sentence. It is manageable. But, IMO, it's better to know.
I was having the exact same symptoms as everyone here. It went on for months. Actually, it's still happening. At first I thought I had BV or a yeast infection, but there was no tell-tale odor or anything of the sort. Two rounds of antibiotics did nothing. So when I found this thread, it was incredibly comforting because it was oddly nice to know I wasn't the only one confused by this. Finally, this month it was the worst ever so I went back to the doctor... which is what brings me here...
I know what this is.
For months I was dealing with the discharge. Like you all said - exactly like wet toilet paper and odorless. Sure, it was annoying as heck, but that's all it was. Discharge. (Which is also why I got treated for BV twice... doc and I both thought it was just an infection.) After a while I noticed that for a few days each month I was getting pretty bloated, and as someone mentioned here, almost as if my digestive system "shuts down" in a way. Then, the bloating... but almost like swelling?... kept getting worse and worse. After a few months of it, each bloating "session" would feel as if I gained 50lbs overnight. One of the biggest clues was that the bloating was always the worst right around the time I should be ovulating. Finally, this month, I ended up face down on my desk in pain trying to explain to my boss that I needed to go to the doctor because this is just not right. My back was on fire. It felt like I did too many situps - with my uterus. My breasts were so swollen that the lightest touch to my nipple would practically put me in tears. This had NEVER happened before, but looking back at the progression of this over the months, it probably shouldn't have been a surprise to me. I guess hindsight is 20/20, ya know?
So I now have a diagnosis - Endometriosis.
I didn't find my treatment options all that desirable. Apparently I can go on birth control so I only have a period 3x per year, but over the years I've become very anti-synthetic drugs. That, and the side effects for the pills included things like heart attack and stroke... I don't know, it just put me off. Also, I could have surgery to remove the tissue, but from what I've been reading, the tissue tends to grow back which would mean multiple surgeries. Hmm, so far, not a fan.
So, I've been digging into a lot of research on this and found that much like fibroids, fibrocystic breast disease, ovarian cysts, ovarian cancer and breast cancer, endometriosis seems to go hand in hand with very high levels of estrogen. Another hindsight I suppose since high estrogen conditions (like those mentioned above) seem to run in my family.
I've decided to treat this for myself I'm going to look into natural ways to lower my estrogen levels. I figure, if need be, the birth control pills are always there as a fallback plan. But, I'm still learning about this myself... if you'd like to get more information, I suggest googling things like "estrogen dominance" and "+endometriosis +estrogen". And the reason I tell you this is because, it might be worth looking into getting your estrogen levels under control before this 'kind of annoying' condition turns into 'face down on your desk in throbbing pain' like mine did. I really wouldn't wish that kind of pain on anyone.
I hope I haven't scared anyone. It's not a death sentence. It is manageable. But, IMO, it's better to know.
Loading...
HI, i have also been having these unusual problems i thought mine might have been from having a urinary track infection and it was reacting to the medicine, but reading all these replies that cannot be it... the burning isnt constant ans neither is the itching but im having to change my panties a couple times a day...?? if your doing the same please give me a soution...
thanks oh so much!!
thanks oh so much!!
Loading...
I want to know what this is too!
I've been self treating myself for a yeast infection and was given a prescription for fluconazole by my dr but it doesn't go away!
My mum has always suffered with similar thrush-like symptoms and hers is due to a lack of estrogen. Could this be the case?
Its not itchy at all but is white or cream like in appearance, in manageable amounts but occasionally (normally mid-cycle) it flares up and I can literally scoop large amounts and my insides seem to be soaking when it gets like this!
I need a cure as it really is starting to ruin my life! I feel i can't have a sexual relationship with my partner because its so embarrassing!
I've been self treating myself for a yeast infection and was given a prescription for fluconazole by my dr but it doesn't go away!
My mum has always suffered with similar thrush-like symptoms and hers is due to a lack of estrogen. Could this be the case?
Its not itchy at all but is white or cream like in appearance, in manageable amounts but occasionally (normally mid-cycle) it flares up and I can literally scoop large amounts and my insides seem to be soaking when it gets like this!
I need a cure as it really is starting to ruin my life! I feel i can't have a sexual relationship with my partner because its so embarrassing!
Loading...
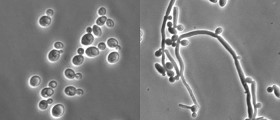
This sounds like what most of you are describing. It's a very common fungus infection.
•Vulvovaginal candidiasis
What is the cause of vulvovaginal candidiasis?
About 20% of non-pregnant women aged 15 to 55 harbor Candida albicans in the vagina. Most have no symptoms and it is harmless to them. Overgrowth of Candida albicans causes a heavy white curd-like vaginal discharge, a burning sensation in the vagina and vulva and/or an itchy rash on the vulva and surrounding skin.
Estrogen causes the lining of the vagina to mature and to contain glycogen, a substrate on which Candida albicans thrives. Lack of estrogen in younger and older women makes vulvovaginal candidiasis much less common.
Overgrowth of Candida albicans occurs most commonly with:
•Pregnancy
•Higher dose combined oral contraceptive pill and estrogen-based hormone replacement therapy
•A course of broad spectrum antibiotics such as tetracycline or amoxiclav
•Diabetes mellitus
•Iron deficiency anaemia
•Immunological deficiency e.g., HIV infection
•On top of another skin condition, often psoriasis, lichen planus or lichen sclerosus.
•Other illness
What are the symptoms?
Symptoms of vulvovaginal candidiasis, i.e., an overgrowth of Candida albicans, include:
•Itching, soreness and/or burning discomfort in the vagina and vulva
•Heavy white curd-like vaginal discharge
•Bright red rash affecting inner and outer parts of the vulva, sometimes spreading widely in the groin to include pubic areas, inguinal areas and thighs.
These may last just a few hours or persist for days, weeks, or rarely, months.
Symptoms may sometimes be aggravated by sexual intercourse.
How is the diagnosis made?
The doctor diagnoses the condition by inspecting the affected area and recognising typical clinical appearance. The pH of the discharge tends to be less than 4.5 the diagnosis is often confirmed by a vaginal swab. In recurrent cases the swab should be repeated after treatment to see whether Candida albicans is still present.
It is best to avoid treatment for four weeks prior to a swab to improve the chance of positive culture.
Swab results can be misleading because the Candida albicans can be present without causing symptoms, and it can only be cultured if a certain amount is present. Swabs from outside the vagina can be negative, even when the yeast is present inside the vagina and there is a typical rash on the vulva. This is because the vaginal discharge has caused an irritant dermatitis, rather than the rash being directly due to infection.
Some women with recurring vulvovaginal symptoms appear to be hypersensitive to the organism (cyclic vulvovaginitis). In these cases it may be difficult for the laboratory to detect the yeast as a vigorous dermatitis has eradicated it.
In other cases, a different species of yeast i.e. a non-albicans candida is found. This is not likely to cause significant vulvovaginitis. Antifungal agents may not clear non-albicans candida from the vagina but luckily, it tends to disappear in time by itself.
Similar symptoms may occur from cytolytic vaginosis.
Treatment
Appropriate treatment for Candida albicans infection can be obtained without prescription from a chemist. If the treatment is ineffective or symptoms recur, see your doctor for examination and advice.
There are a variety of effective treatments for candidiasis. Topical antifungal pessaries or vaginal tablets are usually recommended – in mild cases a single treatment is all that is necessary. A cream formulation may be preferred. Oral antifungal medicines may be used if Candida albicans infection is severe or recurrent.
The creams can be used safely in pregnancy, but the tablets are best avoided.
Not all genital rashes are due to candida, so if treatment is unsuccessful it may because you have another reason for itching (pruritus vulvae) or burning (vulvodynia).
Occasionally Candida albicans infection persists despite adequate conventional therapy. In some women this may be a sign of iron deficiency, diabetes mellitus or an immune problem, and appropriate tests should be done.
It is now thought that women who experience recurrent vulvovaginal Candida albicans do so because of persistent infection, rather than re-infection. The aim of treatment in this situation is therefore to avoid the overgrowth of candida that leads to symptoms, rather than necessarily being able to achieve complete eradication or cure.
There is some evidence that the following measures can be helpful:
•Cotton or moisture-wicking underwear and loose fitting clothing – avoid nylon pantyhose.
•Soaking in a salt bath. Avoid soap – use a non-soap cleanser or aqueous cream for washing.
•Apply hydrocortisone cream to reduce itching and treat secondary dermatitis affecting the vulva.
•Treat with an antifungal cream before each menstrual period and before antibiotic therapy to prevent relapse.
•A prolonged course of a topical antifungal agent is occasionally warranted (but these may themselves cause dermatitis or result in proliferation of non-albicans candida).
•Oral antifungal medication (itraconazole or fluconazole) may be taken regularly and intermittently (e.g. once a month). The dose and frequency is quite variable, depending on the severity of symptoms. Oral antifungal agents may be unsuitable in pregnancy. They require a prescription.
•Boric acid (boron) 600mg as a suppository at night may help to acidify the vagina and reduce the presence of yeasts (albicans and non-albicans candida).
•Vulvovaginal candidiasis
What is the cause of vulvovaginal candidiasis?
About 20% of non-pregnant women aged 15 to 55 harbor Candida albicans in the vagina. Most have no symptoms and it is harmless to them. Overgrowth of Candida albicans causes a heavy white curd-like vaginal discharge, a burning sensation in the vagina and vulva and/or an itchy rash on the vulva and surrounding skin.
Estrogen causes the lining of the vagina to mature and to contain glycogen, a substrate on which Candida albicans thrives. Lack of estrogen in younger and older women makes vulvovaginal candidiasis much less common.
Overgrowth of Candida albicans occurs most commonly with:
•Pregnancy
•Higher dose combined oral contraceptive pill and estrogen-based hormone replacement therapy
•A course of broad spectrum antibiotics such as tetracycline or amoxiclav
•Diabetes mellitus
•Iron deficiency anaemia
•Immunological deficiency e.g., HIV infection
•On top of another skin condition, often psoriasis, lichen planus or lichen sclerosus.
•Other illness
What are the symptoms?
Symptoms of vulvovaginal candidiasis, i.e., an overgrowth of Candida albicans, include:
•Itching, soreness and/or burning discomfort in the vagina and vulva
•Heavy white curd-like vaginal discharge
•Bright red rash affecting inner and outer parts of the vulva, sometimes spreading widely in the groin to include pubic areas, inguinal areas and thighs.
These may last just a few hours or persist for days, weeks, or rarely, months.
Symptoms may sometimes be aggravated by sexual intercourse.
How is the diagnosis made?
The doctor diagnoses the condition by inspecting the affected area and recognising typical clinical appearance. The pH of the discharge tends to be less than 4.5 the diagnosis is often confirmed by a vaginal swab. In recurrent cases the swab should be repeated after treatment to see whether Candida albicans is still present.
It is best to avoid treatment for four weeks prior to a swab to improve the chance of positive culture.
Swab results can be misleading because the Candida albicans can be present without causing symptoms, and it can only be cultured if a certain amount is present. Swabs from outside the vagina can be negative, even when the yeast is present inside the vagina and there is a typical rash on the vulva. This is because the vaginal discharge has caused an irritant dermatitis, rather than the rash being directly due to infection.
Some women with recurring vulvovaginal symptoms appear to be hypersensitive to the organism (cyclic vulvovaginitis). In these cases it may be difficult for the laboratory to detect the yeast as a vigorous dermatitis has eradicated it.
In other cases, a different species of yeast i.e. a non-albicans candida is found. This is not likely to cause significant vulvovaginitis. Antifungal agents may not clear non-albicans candida from the vagina but luckily, it tends to disappear in time by itself.
Similar symptoms may occur from cytolytic vaginosis.
Treatment
Appropriate treatment for Candida albicans infection can be obtained without prescription from a chemist. If the treatment is ineffective or symptoms recur, see your doctor for examination and advice.
There are a variety of effective treatments for candidiasis. Topical antifungal pessaries or vaginal tablets are usually recommended – in mild cases a single treatment is all that is necessary. A cream formulation may be preferred. Oral antifungal medicines may be used if Candida albicans infection is severe or recurrent.
The creams can be used safely in pregnancy, but the tablets are best avoided.
Not all genital rashes are due to candida, so if treatment is unsuccessful it may because you have another reason for itching (pruritus vulvae) or burning (vulvodynia).
Occasionally Candida albicans infection persists despite adequate conventional therapy. In some women this may be a sign of iron deficiency, diabetes mellitus or an immune problem, and appropriate tests should be done.
It is now thought that women who experience recurrent vulvovaginal Candida albicans do so because of persistent infection, rather than re-infection. The aim of treatment in this situation is therefore to avoid the overgrowth of candida that leads to symptoms, rather than necessarily being able to achieve complete eradication or cure.
There is some evidence that the following measures can be helpful:
•Cotton or moisture-wicking underwear and loose fitting clothing – avoid nylon pantyhose.
•Soaking in a salt bath. Avoid soap – use a non-soap cleanser or aqueous cream for washing.
•Apply hydrocortisone cream to reduce itching and treat secondary dermatitis affecting the vulva.
•Treat with an antifungal cream before each menstrual period and before antibiotic therapy to prevent relapse.
•A prolonged course of a topical antifungal agent is occasionally warranted (but these may themselves cause dermatitis or result in proliferation of non-albicans candida).
•Oral antifungal medication (itraconazole or fluconazole) may be taken regularly and intermittently (e.g. once a month). The dose and frequency is quite variable, depending on the severity of symptoms. Oral antifungal agents may be unsuitable in pregnancy. They require a prescription.
•Boric acid (boron) 600mg as a suppository at night may help to acidify the vagina and reduce the presence of yeasts (albicans and non-albicans candida).
Loading...
I agree with what you've posted. I am pretty sure that the discharge is a fungal infection but the issue remains of treatment. I would say to go to a doctor for a formal diagnosis and then get a treatment from the doctor. Does that help?
Loading...