Table of Contents
The kidneys are also responsible for hormone secretions (erythropoietin commonly known as EPO and Vitamin D precursor. In Stage 5 kidney disease, the kidneys lose that function as well, and this results in anemia (since erythropoietin stimulates the bone marrow to produce red blood cells) and osteoporosis and fractures (increased porosity of the bones and decreased mineralization since there is a lack of Vitamin D action). In addition to this, toxic waste products which are supposed to be eliminated by the kidneys (urea, excess electrolytes such as potassium, etc.) accumulate in the blood and cause complications (encephalopathy, seizures, muscle twitching, arrhythmias, etc.)
Understanding Dialysis
In its simplest form, dialysis can be defined as a medical process of removing excess water and waste from the blood. In other words, a dialysis procedure serves to fulfill the role of the kidneys when the latter fail. There are two main types of dialysis: hemodialysis and peritoneal dialysis.
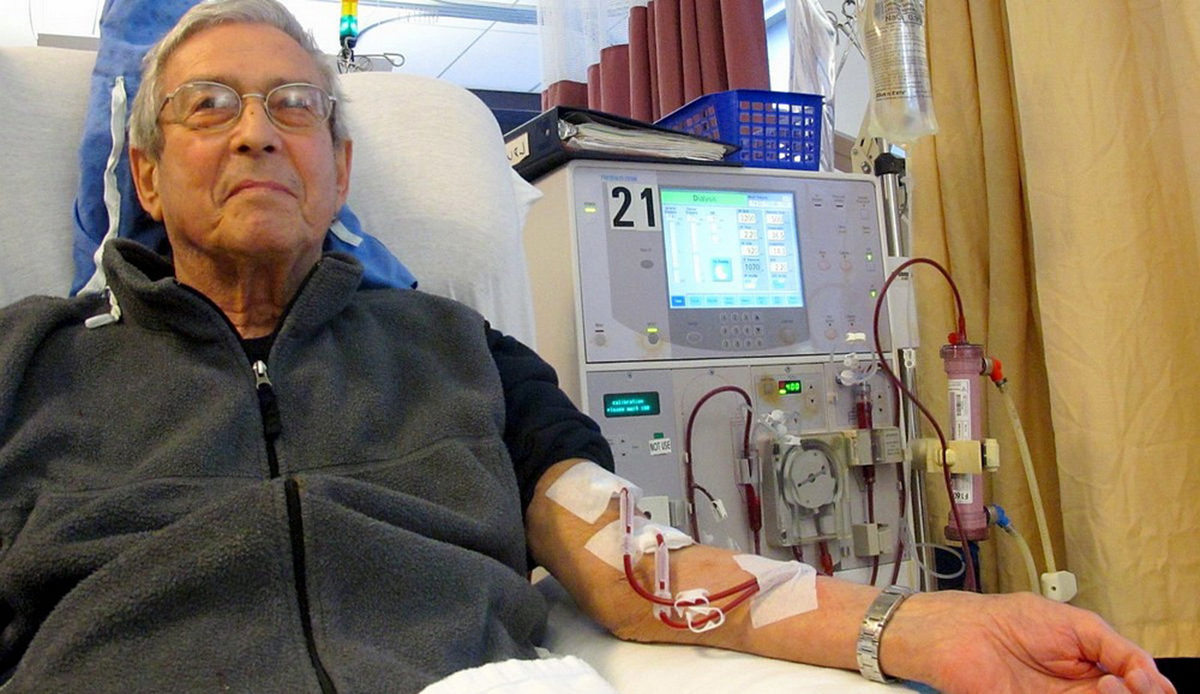
In hemodialysis, the filtration and cleansing process is performed by a dialysis machine. During hemodialysis, the dialyzer is connected to both a vein and an artery. The blood exists the body through the arterial port of the dialyzer, enters the machine and after having been filtered, returns to the body through the venous port.
In peritoneal dialysis, the cleansing and filtration processes are performed via the peritoneal membrane of the abdomen. The peritoneal membrane is a layer of tissue that is made of all the blood vessels that line the abdominal organs (intestines, liver, spleen, etc.). An opening is created in the middle of the abdomen, and a solution containing glucose (called the dialysate) is pushed in the peritoneal cavity. Through the process of osmosis, the waste products are driven from the abdominal organs and vessels to the dialysate solution and emptied in a bag connected outside of the abdominal cavity. Once the bag is filled, it can be removed and changed with a fresh dialysate. This procedure can be repeated 4-5 times a day, and offers the advantage that it can be performed at the patient’s home without any need to move to the hospital or dialysis facility.
See Also: Kidneys Are The Hardest Workers In Your Body
When Does Dialysis Become Necessary?
Dialysis becomes an indication when the patient is diagnosed as having Stage 5 Chronic Kidney Disease. It is also indicated for patients with chronic kidney disease who is experiencing life-threatening complications such as: arrhythmias, seizures, uremic encephalopathy, and pulmonary edema. Dialysis is also used as a temporary measure while waiting for renal transplantation. However, some patients end up going through dialysis for the rest of their life due to the inaccessibility of renal transplantation (donors, fees, etc.) The most common complication of renal dialysis is infections due to catheter use. When a fistula is used, the most common complication is lack of fistula patency.
- Photo by shutterstock.com
- Photo courtesy of Anna Frodesiak by Wikimedia Commons : en.wikipedia.org/wiki/Dialysis#mediaviewer/File:Patient_receiving_dialysis_03.jpg
- http://en.wikipedia.org/wiki/Dialysis#Peritoneal_dialysis
- http://www.renal.org/information-resources/the-uk-eckd-guide/ckd-stages#sthash.GBD1np4a.dpbs
- en.wikipedia.org/wiki/Chronic_kidney_disease#Causes
- www.uptodate.com/contents/indications-for-initiation-of-dialysis-in-chronic-kidney-disease

