Hemochromatosis Type 1 is a hereditary form of this disease, and it causes an excessive absorption of iron from the diet to be stored in the body. Once there is too much iron in the blood, the body is unable to remove it, so it continually builds up, and can affect certain internal organs as well as the joints and skin. Although it is hereditary, the parents may not show any signs or symptoms of the disease, as they are often carriers of the mutated gene but do not have the disease.

Hemochromatosis Type 1: Symptoms
People with hereditary hemochromatosis often don’t show a lot of symptoms, and it is often picked up during routine tests, or when a seemingly minor illness or disorder leads to more investigative procedures. Many often report feeling fatigued, and can have pain in the joints or in the bone. Males are generally not diagnosed until they are in their forties and fifties, and women normally aren't diagnosed until they have gone through menopause. It can affect children, but this is not often seen.
While there are a number of possible symptoms, they can be suggestive of other disorders, and studies have shown that those with an existing liver disease may have an increase in the disease process if they also have hemochromatosis. The main organs that can be affected by hemochromatosis are the liver, the heart and the pancreas. Without treatment, the effects on these organs over a long period of time can be fatal.
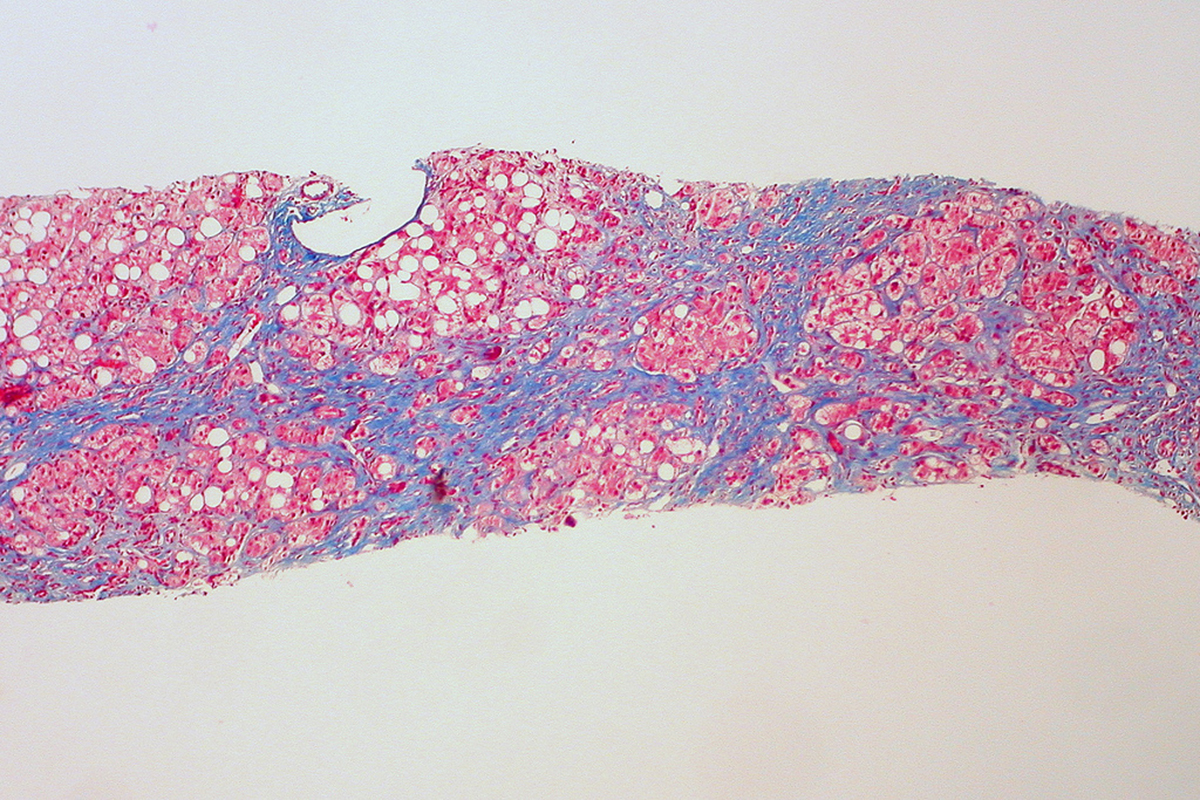
The iron overload can seriously damage the liver. Hemochromatosis can cause cirrhosis of the liver, which is usually seen in alcoholics. Cirrhosis itself can lead to several complications, including liver failure, and there is an increased risk of developing cancer of the liver. The cirrhosis can eventually affect the stomach, the esophagus, the abdomen and the brain.
When the pancreas is overloaded with iron, there is a high risk of developing diabetes mellitus or insulin resistance. The pancreas is responsible for the metabolizing of sugar, but if the iron damages it, the whole process of storing and using sugar becomes compromised. Diabetes itself can be a deadly disease, and often causes many serious complications. Insulin resistance often progresses to diabetes mellitus, and is just as dangerous. Combine this with the liver damage, and it is potentially very life threatening.
See Also: Cold Hands And Feet: The Sign Of Iron Deficiency?
If excess iron accumulates in the heart, it alters the efficiency of blood circulation. This can lead to congestive heart failure, as well as abnormal heart rhythms. Palpitations, arrhythmias and chest pain are all common features of excess iron in the heart. However, if the excess iron is removed, and treatments are followed, this damage can actually be reversed.
Hemochromatosis: Diagnosis And Treatment
Diagnosing hemochromatosis usually occurs as an incidental finding during routine blood tests. If there are elevated liver enzymes, this is a good indicator to check for hemochromatosis. A lot of the time the patient presents with sore or stiff joints, particularly the knees. As well as blood tests, in some cases a liver biopsy may be necessary. This involves the insertion of a fine needle and a tiny sample of the liver tissue being taken. This procedure used to be the only method of diagnosing hemochromatosis, but now it can be done by history, blood screening and presentation instead.
If the liver is enlarged, an MRI may be undertaken to ascertain the size of the liver and what the possible cause may be. When there is an excess of iron in the heart, liver and pancreas, it results in decreased signal intensity in MRI scanning, and degenerative changes in the joints may also indicate hemochromatosis on scanning. The joints of the hands are commonly affected, so these may also be scanned or X-rayed.
One is called African iron overload, once known as Bantu siderosis. However, this typically is only found in those of African descent. The second is called transfusion hemosiderosis, and this can occur in people who have had a number of blood transfusions, especially those with thalassaemia, a condition treated with frequent transfusions. The third is a disease called myelodysplastic syndrome, which effects the production of red blood cells.
Once a diagnosis of hereditary hemochromatosis has been made, it is recommended that the patient’s children, siblings or parents are tested as well. This screening can initiate early treatment and therefore prevent long-term effects of the disease on the body and the organs. Consideration was given to undertaking mass screening of the population in the United States, but it was decided it wasn't necessary due to the low incidence of high iron overload in most.
Hemochromatosis Treatment
The early phase of treatment is done by venesection, which involves draining certain amounts of blood. This is often done weekly in the initial stages until the iron levels reach a healthier level, which is around 20 milligrams per liter. Once that has been achieved, venesection may be done up to 6 times per year to keep the balance of iron healthy. Another option is to use a medicine called desferriioxamine mesilate. This drug is called an iron-chelating compound, and it increases the excretion of the iron, especially when taken in combination with vitamin C. It can’t be used during pregnancy or breastfeeding though, as there is a risk to the unborn child.
See Also: Liver Disease Isn't Just a Danger For Alcoholics
Dietary changes may also help those with hemochromatosis. It is recommended that patients reduce their intake of alcohol and vitamin C. They should also reduce foods that are high in iron such as red meat, shellfish and seafood. Some foods can inhibit iron absorption, and these foods should be increased in the diet. These include calcium, tannin tea, collard greens, and other foods that contain oxalic and phytic acids. These should be eaten at the same time as the foods containing iron to be beneficial.
- Photo courtesy of B Rosen via Flickr: www.flickr.com/photos/rosengrant/3708959626
- Photo courtesy of euthman via Flickr: www.flickr.com/photos/euthman/5517625779

