Table of Contents
Diabetes mellitus has reached epidemic scale these days - it is expected to affect 366 million people by 2030. The impact of this medical condition extends beyond its effects on the body, such as blindness, as its increasing prevalence strongly influences health expenditure and represents a huge economic burden, as translated into loss of productivity and foregone economic growth.
Nowadays, patients have at their disposal a myriad of therapeutics and disease management devices, allowing diabetic people to live a relatively long and healthy life. With this we are starting to see the long term consequences of disease that did not exist in the past because most diabetics did not live beyond their 60th year. At the same time, our knowledge of disease mechanisms and pathophysiology is gradually increasing. As a result of these developments, newer, revolutionary approaches to disease treatment and management have emerged in recent years.
Investigations in the field of nanomedicine (which involves the manufacture, measurement and clinical application of very small (nano)-scale structures), in particular, have yielded very promising results. There are two kinds of great treatment opportunities offered by nanomedicine. One is the miniaturization of existing drug systemsaimed at improving of the biocompatibility and bioavailability of the drug products. The other is more ground-breaking.
This was simply impossible in the recent past.
Nanotechnology may provide better insulin-delivering systems
The first kind includes the nanotechnologies developed for the administration of insulin. Insulin becomes standard therapy for thousands of diabetic patients which do not respond to pills any longer. The invasive multiple injections of precisely calculated amounts of insulin present a significant deterioration of the life quality of diabetic patients. With the aim of addressing this problem, nanomedicine-based alternative routes of administration have been developed. More precisely, nanoparticles, regardless of being produced from natural or synthetic materials, have been shown to effectively pass the inherent barriers for insulin stability, biodegradation, and absorption across gastrointestinal tract and other mucosal membranes, and which, presently, cause the need to administer insulin through injection.
Studies with these new methods of insulin delivery have been conducted with animals and human beings, with a focus on oral and inhaling technologies. However, there are still many obstacles to be surpassed and a lot more research to be done before any of these technologies are available for everyday use by any patient.
Non-insulin-based treatments for pancreatogenic disease
One very specific example of improved delivery of a product for the treatment of diabetes that is not insulin is the one of the pancreatic polypeptide. Pancreatogenic diabetes is a potentially fatal disease that develops subsequently to other pancreatic diseases.
Administration of the pancreatic polypeptide has been shown to be a promising therapeutic option, as this substance improves insulin sensitivity and decreases insulin requirements in pancreatogenic diabetes patients.
See Also: Can Nanomedicine Deliver Miracles In Cancer Treatment?
However, the peptide suffers from the problem of short biological half-life that necessitates continuous administration of the peptide for obtaining therapeutic. Moreover, pancreatic polypeptide has the propensity to aggregate in aqueous media that further complicates effective delivery of this drug. To circumvent this obstacle, a group of researchers of the University of Illinois at Chicago attempted to address the delivery problems of pancreatic polypeptide by associating the peptide with sterically stabilized micelles. Sterically stabilized micelles are polyethylene glycolated (PEGylated) phospholipid micelles that have been shown to increase the half-life of several peptides in vivo, prevent their aggregation in aqueous media and deliver them specifically to desired sites of action in their most active conformation for interaction with cellular targets. A test in diabetic animals revealed that, because of the sterically stabilized micelles, pancreatic polypeptide was delivered to its site of action, effectively improving glucose tolerance and insulin sensitivity.
- REIS, C. P. & DAMGE, C. 2012. Nanotechnology as a Promising Strategy for Alternative Routes of Insulin Delivery. Methods in Enzymology. Elsevier Inc.
- KROLA, S., ELLIS-BEHNKEB, R. & MARCHETTI, P. 2012. Nanomedicine for treatment of diabetes in an aging population: state-of-the-art and future developments. Nanomedicine: Nanotechnology, Biology, and Medicine, 8, S69-S76
- ZHI, Z.-L., KHAN, F. & PICKUP, J. C. 2013. Multilayer nanoencapsulation: A nanomedicine technology for diabetes research and management. Diabetes Research and Clinical Practice, 100, 162-169
- MEETOO, D. & LAPPIN, M. 2009. Nanotechnology and the future of diabetes management. Journal of Diabetes Nursing, 13, 288-297
- Hanazaki K et al. (2001) Artificial endocrine pancreas. J Am Coll Surg 193, 310-322
- Heo YJ and Takeuchi S (2013) Towards smart tattoos: implantable biosensors for continuous glucose monitoring. Adv Healthc Mater 2(1), 43-56.
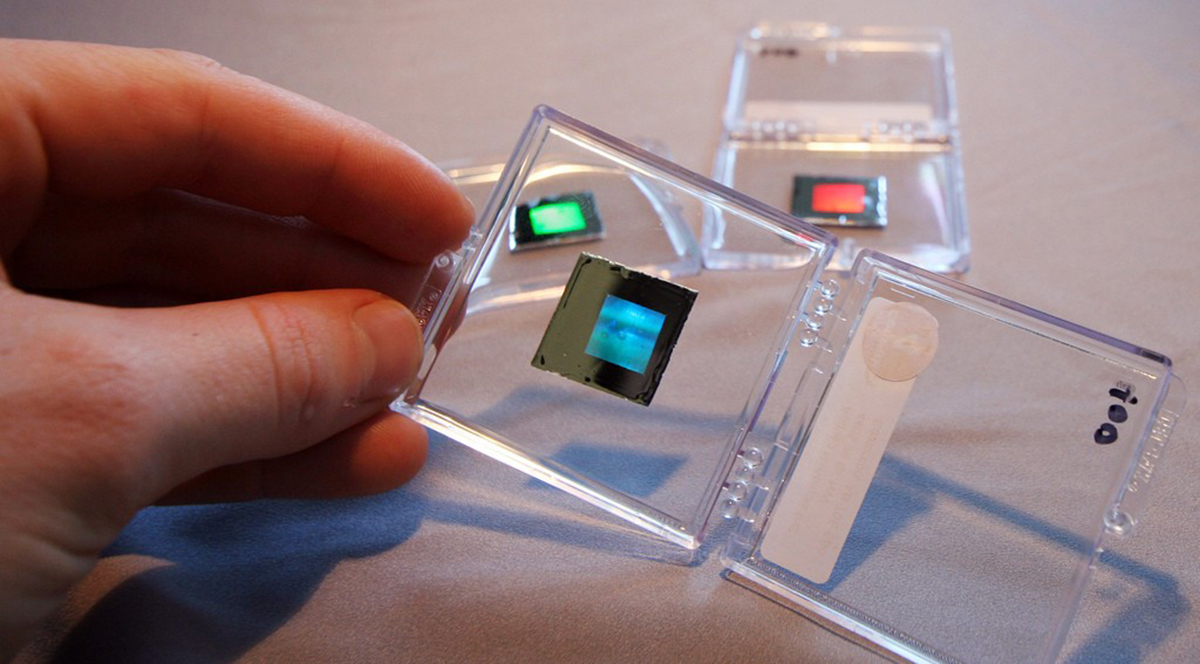
- Photo courtesy of Simon Fraser University Public Affairs and Media Relations by Flickr : www.flickr.com/photos/sfupamr/5355316833
- Photo courtesy of Steve Jurvetson by Flickr : www.flickr.com/photos/jurvetson/149332018


Your thoughts on this