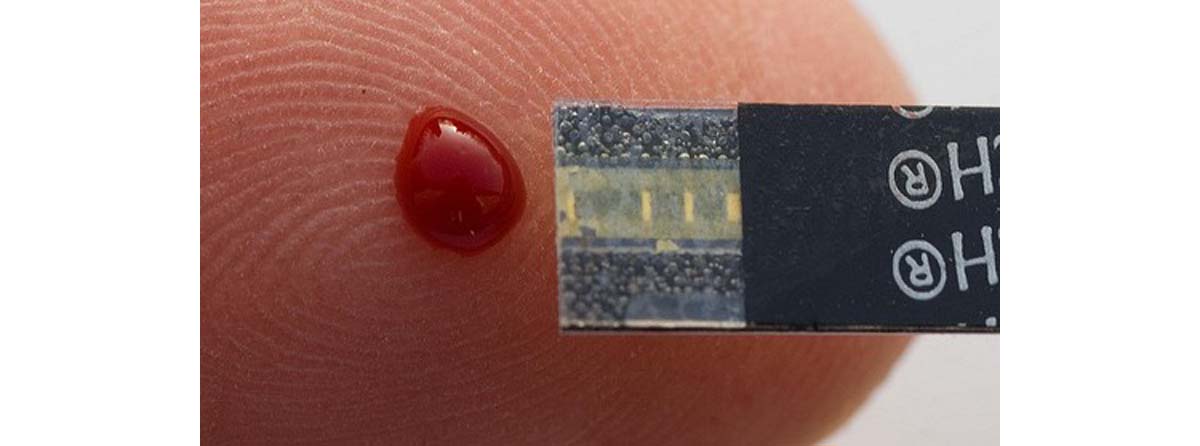
Haematology is a discipline in medicine that focuses on the study, prevention, diagnosis and treatment of conditions and illnesses that affect blood and the production of blood and its components such as haemoglobin, white blood cells, platelets, bone marrow, blood proteins, the spleen, the blood vessels, clotting factors and the mechanisms of coagulation.
Haematologists will consult with patients of all blood-related conditions, but there are those who will sub-specialise in heamato-oncology where they will provide treatment for the types of cancers that affect blood and its components.
Training
In order for a doctor to become a qualified haematologist, they will have to obtain their undergraduate medical degree that qualifies them as a medical doctor and it takes 5-6 years to complete. Thereafter they will have to take part in a mandatory internship training programme, that takes 1-2 years to complete, where the newly qualified doctor is exposed to the numerous medical and surgical disciplines that exist.
The doctor will then be allowed to specialise where they will have to complete a 4 year residency programme in internal medicine, and this will be followed by a fellowship training programme in haematology that takes 2-3 years to complete. It can therefore take a doctor between 12-15 years to become a qualified haematologist.
Conditions managed by Haematologists
Nutritional anaemias
- Iron deficiency anaemia.
- Pernicious anaemia (vitamin B12 deficiency).
- Megaloblastic hereditary and megaloblastic nutritional anaemia.
- Folate deficiency anaemia.
- Transcobalamin 2 deficiency anaemia.
- Protein deficiency anaemia.
- Scurvy due to vitamin C deficiency.
Non-nutritional anaemias
- Acute post-haemorrhagic anaemia.
- Acanthocytosis.
- Alpha-thalassaemia.
- Beta-thalassaemia.
- Anaemia of chronic diseases due to a chronic inflammatory response.
- Autoimmune haemolytic anaemia.
- Aplastic anaemia.
- Anaemia due to chronic kidney illness.
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency anaemia.
- Haemolytic anamia.
- Hereditary anaemia.
- Rhesus deficiency syndrome.
- Sickle-cell anaemia.
Lymphomas
- Hodgkin's lymphoma.
- Non-Hodgkin's lymphoma.
- Hepatosplenic T-cell lymphoma.
- Angioimmuloblastic T-cell lymphoma.
- B-cell lymphoma.
- Diffuse large B-cell lymphoma.
- Intravascular large B-cell lymphoma.
- Follicular lymphoma.
- Burkitt's lymphoma.
Leukaemias
- Acute myeloid leukaemia (AML).
- Acute lymphocytic leukaemia (ALL).
- Chronic myeloid leukaemia (CML).
- Chronic lymphoblastic leukaemia (CLL).
- Polycythaemia vera.
- Hairy cell leukaemia.
Myelomas
- Multiple myeloma
- Myelomatosis.
- Plasma cell leukaemia.
Malignant immunoproliferative diseases
- Monoclonal gammopathy.
- Lymphoid granulomatosis.
- Alpha heavy chain disease.
- Gamma heavy chain disease.
Haemorrhagic conditions and coagulopathies
- Thrombocytosis.
- Disseminated intravascular coagulation (DIC).
- Haemophilia A, B and C.
- Thrombocytopaenia.
- Recurrent thrombosis.
- Idiopathic thrombocytopaenic purpura (ITP).
- Thrombotic thrombocytopaenic purpura (TTP).
- Factor V Leiden.
- Protein C deficiency.
- Protein S deficiency.
- Antiphospholipid syndrome
- Von Willebrand disease.
READ 8 Things They Won’t Tell You about Medical School
Infective conditions
- Malaria (Plasmodium infection).
- E. coli 0157:H7 infection.
- Clostridium infection.
- Typhoid fever.
- Cholera infection.
- Toxoplasmosis.
- Leishmaniasis.
Immune-related conditions
- Hereditary hypogammaglobulinaemia.
- Immunodeficiency with increased immunoglobulin M (IgM).
- Non-familial hypogammaglobulinaemia.
- Selective deficiency of immunoglobulin A (IgA), immunoglobulin M (IgM) and immunoglobulin G (IgG) subclasses.
- Transient hypogammaglobulinaemia of infancy.
- Antibody deficiency with near-normal immunoglobulins or with hyperimmunoglobulinaemia.
The Daily Schedule Of A Haematologist
A haematologist will consult with and manage patients in the hospital on a daily basis and will continue to provide medical care for these patients until they are clinically stable enough to be discharged home. Patients that are seen by these specialists, at times, don't have a good prognosis and they do get to a stage where they will have to be transferred to step-down and hospice facilities where they will receive palliative care.

Haematologists provide on call services for the hospital they work at during after hours and weekends. These specialists will consult with emergency patients who are known with leukaemias and present with persistent high fevers, and patients with severe symptoms of nutritional or hereditary anaemias that need an urgent blood transfusion.
Monday
Mondays are usually administrative days and these aspects are dealt with in the morning after ward patients have been seen, but before out-patients are consulted. These administrative tasks will include confirming and attending meetings with staff, hospital management and medical representatives for the week.
The haematologist will thereafter begin consulting with patients. These patients may be managed conservatively with medication being prescribed for them, they can be sent for further blood work to be done on them which will be followed up and discussed with the patient or they may be admitted to the hospital ward for further investigations to be done and management to be initiated.
Patients with conditions such as acute lymphocytic leukaemia will need to be isolated, and they will then be admitted to the haematology isolation rooms that are specifically built to manage these conditions. Doctors and family visiting these patients need to take preventive measures and wear protective gear to prevent them from transmitting possible pathogens to these patients.
Tuesday
The haematologist will consult with patients in the morning and then spend the afternoon in the haematology laboratory. Here, the specialist will analyze blood specimens, sent by referring physicians, under a microscope and report on their findings which are then sent back to these doctors.
Wednesday
The specialist will once again see their out-patients in the morning. The afternoon will be reserved for performing procedures such as taking bone-marrow biopsies on patients. This will usually be done under local anaesthetic but may need to be done in theatre under general anaesthesia depending on the patient.
READ Questions To Ask Yourself When Wanting To Study Medicine
The afternoon may be used for giving feedback to patients regarding their investigative results, filling in of chronic prescriptions and motivation letters to the medical insurance companies or for doing further research for the specialists own academic needs.
Thursday
Th haematologist will continue to manage their patients in the ward and will then move on to seeing outpatients in their offices. The afternoon will be used for training of medical undergraduate students and postgraduate clinical assistants specialising in internal medicine or haematology.
A lot of haematologists will be affiliated with an academic institution since a lot of research is done at these facilities and patients are usually involved in clinical trials of oncological and haematological medications.
Friday
The haematologist will consult with patients again in the mornings and the afternoons will be used for finalising unfinished administrative tasks. The work week can then be concluded once all patients have been seen and the administrative issues have been dealt with.
Haematologists who are on call for the weekend will be looking after their own patients, as well as those who are discussed with by their colleagues.
- en.wikipedia.org/wiki/Hematology
- en.wikipedia.org/wiki/List_of_hematologic_conditions
- Photo courtesy of tyfn: www.flickr.com/photos/tyfn/8057597193/
- Photo courtesy of shutterstock.com
- Photo courtesy of tyfn: www.flickr.com/photos/tyfn/8057597193/


Your thoughts on this