Table of Contents
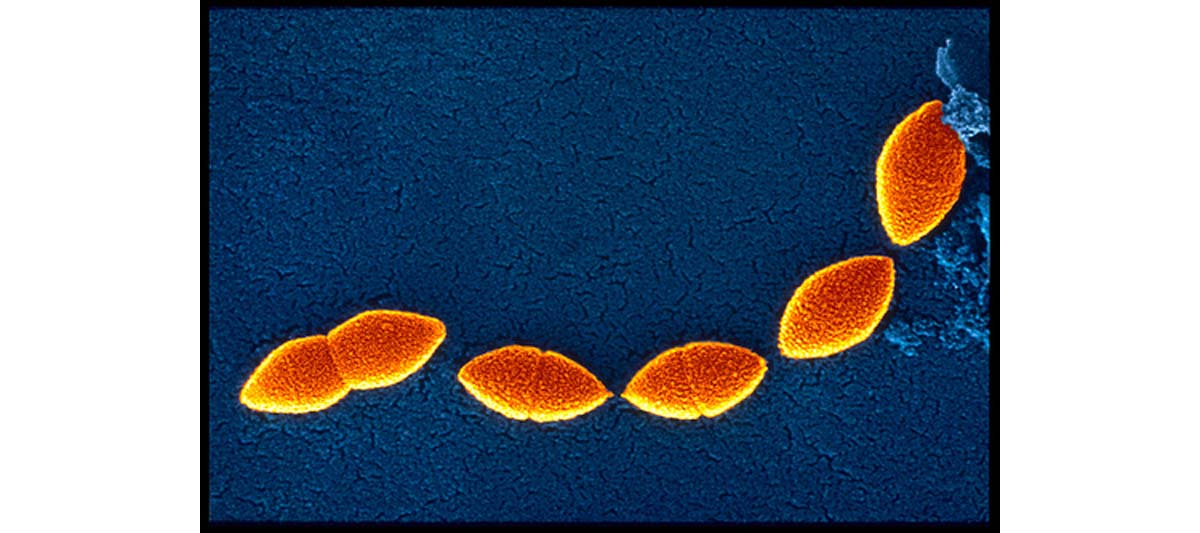
Septic shock is a potentially lethal drop in blood pressure due to the presence of bacteria in the blood. This condition, characterized by the presence of bacteria in blood, is also called the bacteremia.
Like we have already mentioned, the severe sepsis is characterized by stimulation of a series of inflammatory cascades leading to extensive cardiovascular problems and the most obvious signs are hypotension due to vasoplegia, relative hypovolemia, and widespread dysfunction of the microvasculature. That’s why; the two major priorities in management of septic patients are
- To maintain delivery of oxygen to the tissues, by way of optimization of cardiac output and peripheral resistance, and
- To modulate the procoagulation response
Recommended antibiotics in septic shock
Suspected source
Recommended antibiotics
Pneumonia
Second- or third-generation cephalosporin plus macrolide (antipseudomonal beta lactam plus aminoglycoside if hospital-acquired)
Urinary tract
Ampicillin plus gentamicin (Garamycin) or third-generation cephalosporin
Skin or soft tissue
Nafcillin sodium (Nafcil, Nallpen, Unipen) (add metronidazole [Flagyl, Metro IV, Protostat] or clindamycin if anaerobic infection suspected)
Meningitis
Third-generation cephalosporin
Intra-abdominal
Third-generation cephalosporin plus metronidazole or clindamycin
Primary bacteremia
Ticarcillin and clavulanate potassium (Timentin) or piperacillin sodium and tazobactam sodium (Zosyn)
Possible complications
Significant complications from sepsis include:
· central nervous system dysfunction
· adult respiratory distress syndrome (ARDS)
· liver failure
· acute renal failure (ARF
· disseminated intravascular coagulation (DIC)
Prognosis
Every patient should know that the chanced for recovery from septic shock depend on several factors and the most important including:
· the degree of immuno-suppression of the patient
· underlying disease
· promptness of treatment,
· Type of bacteria responsible.
Prevention
Like we have already mentioned- several researches done in the past have shown that septic shock is most likely to develop in the hospital, since it follows infections which are the primary form of this condition. That’s why; in order to prevent this it is crucial to know that careful monitoring and early, aggressive therapy can minimize the possible likelihood of progression. It is logical to assume that the risk of developing septic shock can be minimized through treatment of underlying bacterial infections, and prompt attention to signs of bacteremia.

