UPDATE: April 17th 2011
I had a colonoscopy in early 2010 due to blood in my
stool. It turned out to be hemorrhoids. The doctor stated that I was "squirming
through the procedure," and that I "nearly jumped off the table"
at one point. As soon as I woke up, I
had pain in my left side, under the bottom left rib. The pain persisted, I went
back to the doctor and they recommended I get a CT scan and blood work. Everything came back normal. It was then stated I should I have an
endoscopy. I then had an endoscopy with
another doctor, it too, the initial results were normal while the biopsies were
sent to pathology. The doctor then stated "there is nothing else I can do
for you." I have never had pain in my left abdominal area, until the
colonoscopy. The tests were normal. I do not feel sick, I do not have any blood
in the stool or any other symptoms at this time.
Not sure where to go, I decided to see some surgeons about the issue. One surgeon recommended I get a HIDA scan with CCK, even though my pain was in the LUQ. Prior to the test, I have never had pain on my right side. After the scan, I had RUQ pain for awhile constantly, it did go away somewhat; however, if I twist or contort my body the right side hurts. When I spoke to the surgeon about it, he said he has never heard of anyone having RUQ pain constantly after a HIDA/CCK. So now I have LUQ pain from the colonoscopy (and RUQ pain from the HIDA/CCK if I put pressure where my gallbladder is located). The ejection fraction was 22% it was low; however, from the many (6) surgeons I have seen, four say they would not want to remove the gallbladder, while the other two (part of the same group) want to remove the gallbladder.
Has anyone else had a HIDA/CCK test and then have RUQ pain afterwards? Can a HIDA/CCK test kill a gallbladder, or overwhelm a failing one?
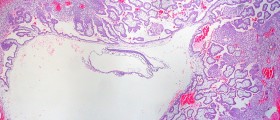
One or two months later after the pathology came back
from the endoscopy, the pathology revealed I have chronic gastritis, I've never
had any LUQ pain before in my life, prior to the colonoscopy. In addition, I also had blood work to test
for H. Pylori, it was negative. Now,
more than 1 year later, the gastritis continues, in addition, sometimes when I
bend over to tie my shoes or if I lie on my left side at 'just the right angle'
I will feel stabbing pains on the left side, even when taking PPIs for the
gastritis. I've asked for a diagnostic
laparoscopy but surgeons seem to be reluctant to perform the procedure. If you were in this situation what would you
do?
Would you have your gallbladder removed and while in there, they could look at the left upper quadrant? Or try to find a surgeon (out-of-state?) who would perform a diagnostic laparoscopy? I'd hate to get the gallbladder removed and have both the LUQ and RUQ pain remain or get worse; however, I am very tired living with this pain, aside from work, I do not want to go anywhere, do anything or meet anyone, it is ruining my life. What would you do in my situation?
Loading...
Good: Recently, I had a diagnostic laparoscopy and an adhesion was found between the colon and the lateral abdominal wall, it was removed and the painful, sharp stabbing pain is now gone.
Bad: Due to the HIDA+CCK scans last year (for the LUQ pain), I still have RUQ pain under the right rib cage; on a scale from 1-10 it is generally a 0-1 while sitting and 4-6 if I lay on my right side, depending on the angle. When jogging, after 1-2 miles the pain will shoot up to 8-9 and 10 if I have to stop running because of it. I’ve had almost every scan and test one can think of: CT, MRCP, EUS, VQ LUNG SCAN ENDOSCOPY, SECOND COLONOSCOPY, ULTRASOUND, all results came back normal. My RUQ does not hurt if I eat fatty foods. From what I can deduce it is either my liver or gallbladder causing this pain. Running out of options, I also went to an acupuncturist, recommended by my PCP; he said my liver was “tight.” I do not drink or smoke and am desperately looking for thoughts or ideas that could lead me to a solution.
Does anyone have _any_ thoughts at all what could be causing this RUQ pain?
Recall:
1. The first CCK injection (which caused EXCRUCIATING pain and then burning for 3-4 weeks after; was injected in 30 seconds) @ 22% ejection fraction rate.
2. The second CCK injection (a few months later) was done by a different nurse/technician who had been doing this procedure for ~20 years; she had stated that 30 seconds was too fast and a normal injection is done over a period over 2 minutes, which is how she did it and the ejection fraction was 56% and I had no pain.
Current situation:
1. With the LUQ pain; prior to the colonoscopy I never had any pain, it turned out to be an adhesion stuck between the colon/lateral abdominal wall, no scan or test showed this problem, it was only at the last resort of surgery that found and removed the adhesion.
2. With the RUQ pain; prior to the HIDA+CCK scan, I never had any pain, I've had almost every test (except ERCP which carries a lot of risk) and the pain has not gone away. During the laparoscopy the RUQ of the abdomen was also searched and no problems were found.
Can anyone offer any suggestions or insight into this issue?
Loading...
Loading...
Further tests showed that I have gastritis and duodenitis and I have pain when I eat no matter what it is in the stomach and RUQ pain persists, I have not found a solution yet, I am still looking.
Have you had an endoscopy to rule out stomach issues?
Additionally, you have RUQ pain after your HIDA scan that never went away?
If you do not eat anything, do you still experience the abdominal pain?
The only thing I can think of at this point is the tissue is inflamed due to what was noted above but I am not sure how to make it go away..
Loading...