The incidence of appendicitis — a painful inflammation of the appendix — is lower in cultures with a higher intake of dietary fiber as part of their normal nutrition. Dietary fiber decreases the viscosity of feces, decreases bowel transit time, and discourages the formation of feces that predispose individuals to obstructions of the appendicle lumen. Considering the dangers appendicitis could provoke, it very important to know how to recognize the signs of acute appendicitis.
What Is The Appendix?
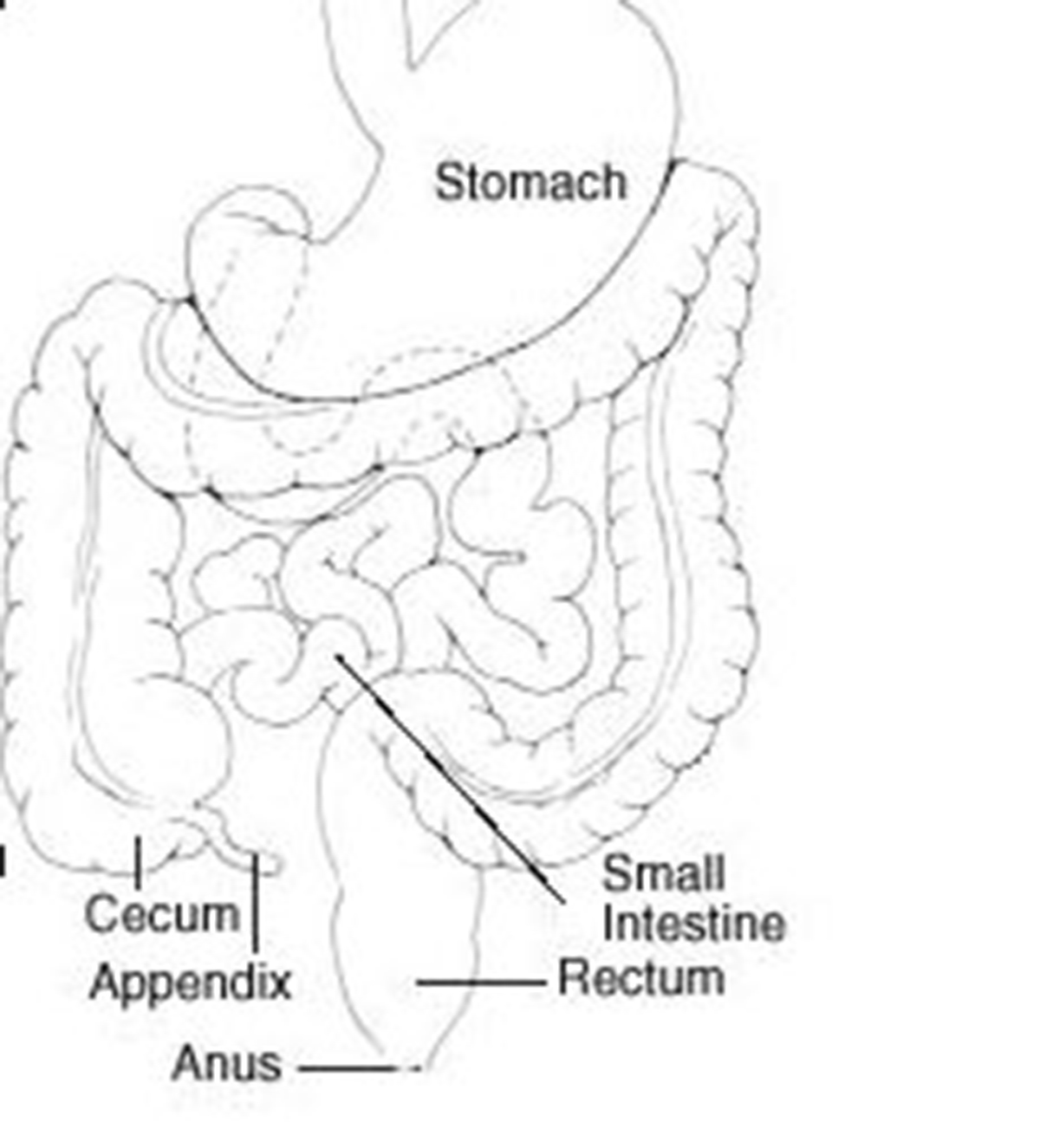
The inner lining of the appendix produces a small amount of mucus. This mucus flows through the appendix and into the cecum. The wall of the appendix contains lymphatic tissue that is a part of the immune system responsible for making antibodies.
Like the rest of the colon, the wall of the appendix also contains layers of muscles. In adults, the appendix averages 10 cm in length. However, the appendix can range in length from 2 to 20 cm. The diameter of the appendix is usually less than 7-8 mm. While the base of the appendix is at a constant location, the location of the tip of the appendix can vary. Usually, it varies from being retro-caecal to being in the pelvis to being extra-peritoneal. In most cases, the appendix is located in the lower right quadrant of the abdomen. [1]
The real function of the appendix remains a controversial point in the field of human physiology. Hypothesized functions for the appendix include lymphatic, endocrine, exocrine, and neuromuscular functions. However, most physicians believe the appendix lacks any significant function, and that it exists primarily as a vestigial remnant of the larger cellulose-digesting cecum — a part that lost its function with human evolution.
What Is Appendicitis?
Appendicitis is an inflammation of the appendix, beginning when the opening from the appendix into the cecum becomes blocked.
The blockage may develop as a result of a build-up of thick mucus within the appendix. It could also be blocked with stool that enters the appendix from the cecum. The mucus or stool that hardens, becomes rock-like, and blocks the opening, is called a fecalith. This literally means “a rock of stool”.
In other cases, the lymphatic tissue in the appendix may swell and block the appendix. Bacteria that are normally found in the appendix then begin to invade the wall of the appendix. The body will respond to this bacterial invasion by mounting an attack on the bacteria in the form of kick-starting an inflammatory process. [1]
If the inflammation and infection spread through the wall of the appendix, the appendix can rupture, so the infection can spread throughout the abdomen. In advanced stages of inflammation when the wall of the appendix begins to break down, gangrenous, perforated, or ruptured, appendicitis can occur.
Symptoms Of Appendicitis
There are several main symptoms of appendicitis, but they differ from person to person [2]:
- Abdominal pain is at first diffuse (spread over a wider area), poorly localized, and not confined to one spot. The pain is so difficult to pinpoint that when asked to point to the area of the pain, most people cannot exactly indicate the location. Once the peritoneum becomes inflamed, the nature of the pain changes and then can be localized clearly to one small abdominal area. Generally, this area is between the front of the right hip bone and the belly button of the patient. The exact point is known as McBurney's point. If the appendix ruptures and the infection spreads throughout the abdomen, the pain diffuses again as the entire abdomen becomes inflamed.
- Nausea and vomiting accompany appendicitis and may be due to intestinal obstruction.
- Progressive tenderness in the right lower abdomen follows coughing or trying to move about.
- Loss of appetite is also a common symptom of acute appendicitis.
- Fever tends to appear but is usually not very high.
- Elevated white blood cell count is a symptom found in diagnostic studies as well.[3]
Other potential signs and symptoms of acute appendicitis may include [3]:
- Abdominal pain near the navel in the earliest stages
- Right-sides abdominal pain in later stages
- Abdominal pain during activity
- Abdominal pain when breathing
- Abdominal pain when coughing
- Abdominal pain when sneezing
- Abdominal sensitivity when touching the area
Other signs of appendicitis might include constipation, diarrhea, loss of appetite, an inability to pass gas, low fever, abdominal swelling, and bad breath.
In some cases, the symptoms of appendicitis are not clear-cut, and appendicitis becomes difficult to diagnose. Pain may not start in the mid-abdomen or belly button region and tenderness may not be prominent.
Diagnosing Acute Appendicitis
The diagnosis of appendicitis begins with a thorough history and physical examination of the patient. Patients often have an elevated temperature (fever), and moderate to severe tenderness in the right lower abdomen when pressure is applied.
If the inflammation has spread to the peritoneum, there is frequently rebound tenderness. This means that when the doctor pushes on the abdomen and then quickly releases their hand, the pain becomes suddenly and transiently worse.
- White blood cell count usually becomes elevated with an infection. In early appendicitis, before severe infection sets in, the white blood cell count can be normal, but most often there is at least a mild elevation. Unfortunately, appendicitis is not the only condition that causes an elevated white blood cell count; any infection or inflammation can cause this count to be abnormally high. Therefore, an elevated white blood cell count alone cannot be a sure sign of appendicitis. [3]
- Urinalysis is a microscopic examination of the urine that detects red blood cells, white blood cells, and bacteria in the urine. Urinalysis is abnormal when there is inflammation or stones in the kidneys or bladder. These conditions can be confused with appendicitis sometimes. Therefore, an abnormal urinalysis suggests that a person may be dealing with a kidney or bladder problem, but a normal urinalysis is more characteristic of appendicitis. [4]
- An abdominal X-Ray may detect the presence of a fecalith, which is a hardened and calcified, pea-sized piece of stool that blocks the appendiceal opening. This cause of appendicitis is especially common in children. [5]
- Ultrasound is a painless procedure that uses sound waves to identify organs within the body. Ultrasound can identify an enlarged appendix or abscess. When a patient has appendicitis, doctors are able to see the appendix using an ultrasound in only 50% of patients. Therefore, not seeing the appendix during an ultrasound does not exclude appendicitis as a diagnosis, and CT scan has a better diagnosis rate if the results of an ultrasound scan remain inconclusive. [6]
- Barium enema is an x-ray test where doctors enter liquid barium through the anus into the colon. This test can, at times, show an impression on the colon in the area of the appendix from the adjacent inflammation. The use of the barium enema in the diagnosis of appendicitis is useful in patients with an atypical clinical presentation. [7]
- A CT scan of the area of the appendix is useful in diagnosing appendicitis and peri-appendiceal abscesses. A CT scan is also useful in excluding other diseases inside the abdomen and pelvis that can mimic appendicitis, bringing the doctor closer to an accurate diagnosis. [6]
- Laparoscopy is a surgical procedure wherein a small fiber-optic tube with a camera is inserted into the abdomen through a small puncture made on the abdominal wall. Laparoscopy allows a direct view of the appendix as well as other abdominal organs. In most laparoscopic appendectomies, surgeons operate through 3 small incisions (each ¼ to ½ inch) while watching an enlarged image of the patient’s internal organs on a television monitor. In some cases, one of the small openings may be lengthened to complete the procedure. [8] If appendicitis is present, the inflamed appendix can be removed at the same time. The disadvantage of laparoscopy compared to ultrasound and CT scanning is that the procedure requires the patient to have a general anesthetic.
Test For Appendicitis
Since there is no one test able to diagnose appendicitis, the approach to suspected appendicitis may include a period of observation, tests as previously discussed, or surgery.
It is also possible to have a drop test. The patient suspected of having appendicitis has to stand on the tip of their toes and drop to the heels. This sends a sharp pain to the area where the appendix is located, and confirms appendicitis. [9]
This method, as well as push tests and rebound tenderness, should be avoided in modern medicine because they can cause the appendix to rupture. Instead, pushing on the opposite side of the abdomen, and then quickly removing fingers works as well. The patient should feel pain over the area of the appendix, without having it actually touched.
Read More: Appendix removal: When is Appendectomy really needed?
Acute Appendicitis Treatment
The treatment of acute appendicitis starts only when the diagnosis is clear.
Most commonly, appendicitis treatment involves surgically removing the inflamed appendix in an operation known as an appendectomy [8]. An appendectomy is a routine surgery, considered to be very safe when the appendix has not ruptured yet.
During the operation, the doctor will make a small incision in the right lower abdomen (or by use of laparoscopic instruments in selected patients). If the appendicitis is uncomplicated, which means it is not associated with an abscess or perforation, the patient is able to go home as soon as 24 to 48 hours after the operation.
Other noted advantages of an laporascopic appendectomy are [8]:
- Less postoperative pain
- Shorter hospital stay, as already mentioned
- A quicker return to bowel function
- A quicker return to normal activity
- Better cosmetic results
Because health care providers cannot always be sure that the appendix is inflamed until they examine the organ during surgery, about 10% of removed appendixes were not inflamed, and the cause of the patient's symptoms turned out to be a problem other than appendicitis. If a patient has had surgery and the appendix was normal, the doctor is going to remove it anyway, while other possible causes of abdominal pain will be looked for. It is appropriate for a surgeon to risk the removal of a normal appendix.

