More Antibiotic-Resistant Strains of Bacteria Appearing in More Places
At first, MRSA was only a problem in hospitals but nowadays it is found in gyms, nursery schools, and retirement centers. Sometimes healthy people pick up MRSA infections through cuts and scrapes. The dangerous aspect of MRSA is that it has the ability to survive despite exposure to methicillin, the antibiotic given to people with life-threatening infections when other antibiotics fail.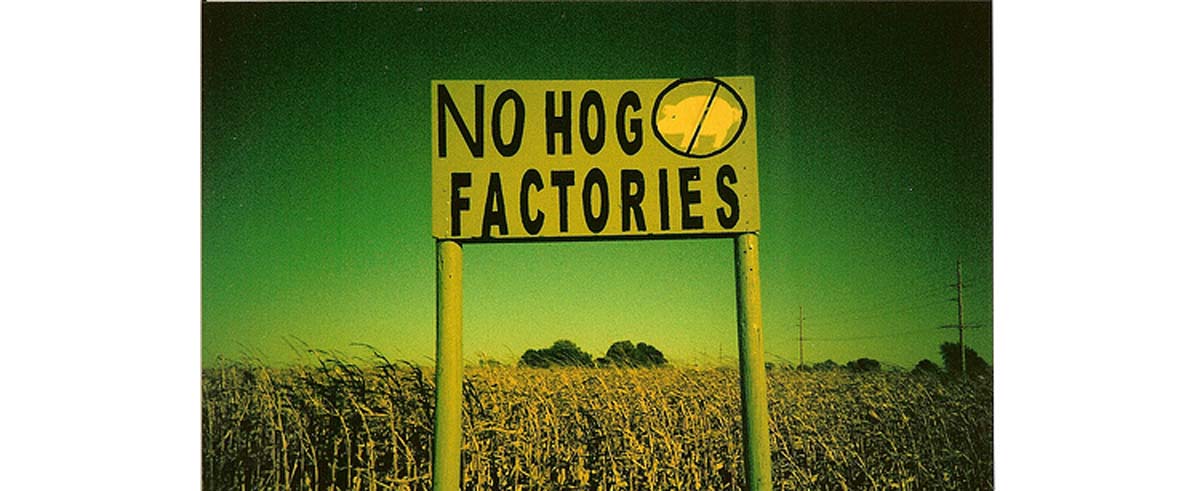
Antibiotic resistance is literally a deadly, serious concern. Even healthy people can become infected with "super bugs" that cannot be treated, death sometimes striking an active, healthy person in just hours. Or even worse, the immune system may resist the infection leading to weeks of agonizing fever, bloating, inflammation, and sepsis before death occurs.
I have to admit a bias on this topic. Both my father and my grandfather died of infections with antibiotic-resistant bacteria, my grandfather of E. coli, and my father of Vancomycin-resistant Enterococcus.
Both had been active, involved senior citizens until they got their infections. Both suffered horribly for months before they eventually died. Describing the actual effects of these infections is still a little too close to me for accurate reporting, but suffice it to say you don't want to get them.
How Bacteria Develop Antibiotic Resistance
Before the 1980's, most antibiotics killed most bacteria. Since the 1980's, doctors are constantly having to introduce new antibiotics to keep infections under control. The way the first bacterium survives an antibiotic treatment is sheer luck. Something causes a mutation in the bacterial DNA.
That mutation leaves one bacterium standing when the treatment is done. If it is destroyed by the immune system, or it is killed by conventional antiseptic treatment, or if it just runs out of food before it divides, that gene does not give any other bacteria the power of antibiotic resistance.
But bacteria can pass genes to others of their species, and even different species, without reproducing. There are several different ways:
- A bacterium can be infected with a virus. The virus latches on to the antibiotic resistance gene and carries it to another bacterium. This process is called transduction.
- A bacterium can rub up against another bacterium and exchange DNA. Although not, strictly speaking, sex, this process allows bacteria to share antibiotic resistance with other microbes. This process is called conjugation.
- And a bacterium can feed on DNA from dead, antibiotic-resistant bacteria, incorporating their genes into its DNA. This process is called transformation. It was first observed in the 1920's by a British biologist named Frederick Griffith. He observed that he could kill a virulent (symptom-causing) strain of Streptococcus pneumoniae and then put the dead, disease-causing bacteria into a live, usually harmless strain of the same bacteria. The usually harmless strain would become a disease-causing strain after coming in contact with dead bacteria.
These processes have been around for millenniums. Why is antibiotic resistance becoming such a major problem now? Some experts believe the culprit is the overuse of antibiotics in livestock feed.
Antibiotic Resistance Caused by Indiscriminate Use in Animal Feeds
Before 1980, most cases of antibiotic resistance were first noticed in New York City hospitals. The USA led the world in antibiotic use, and New York City had the greatest concentration of patients. It was only natural that antibiotic resistance would happen in Manhattan first. Because this pattern was predicable, the spread of the resistant bacteria was easier to contain.
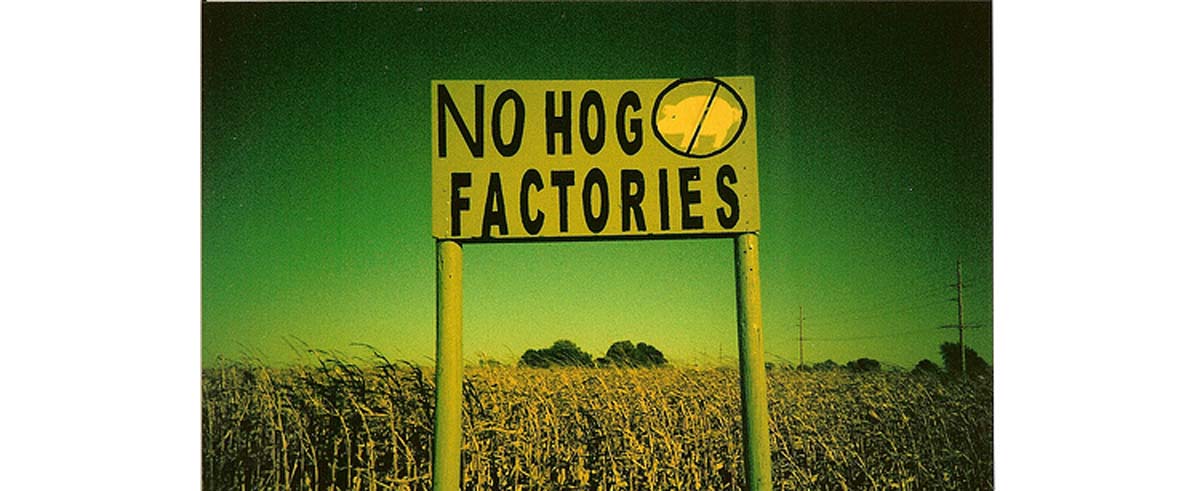
But the source of the bugs that find their way into hospitals all over the world is farms. Antibiotics in animal feeds are just beginning to be used in India and Pakistan. They are much more common in Europe and the USA.
Although some European countries ban antibiotics in animal feed, about 50% of all the antibiotics used in Europe are put in farm animals' feed to prevent infections they don't yet have. About 70% of all the antibiotics used in the USA are bought for this purpose.
Even organic farmers in the USA may use antibiotics, although they will separate animals away from the rest of the herd and not label the meat "organic." In many cases, antibiotic treatment is simply compassionate care. If a cow cuts her udder while jumping over a fence, or a goat eats wire, an injection of antibiotics may save it a great deal of suffering.
On the other hand, dumping antibiotics into feed is all about hoping for a few extra pounds for a few extra pennies for a few thousands or tens of thousands or even millions of animals in a feedlot system. These antibiotics stop the little infections farmers never notice and help animals pack on more fat before slaughter.
More exposure to antibiotics creates more opportunities for antibiotic bacteria to appear and spread. And since some feedlot owners literally feed animals their own waste, antibiotic-resistant strains of bacteria are inevitable. They "jump" from the feedlot to the human population through unsanitary meat processing or manure on boots, which is something you see tracked into restaurants in a few places in the United States that I won't name here. Shortcuts in personal hygiene and shortcuts in restaurant hygiene also spread these potentially deadly infections.
What can you do about antibiotic resistance? Well, if you happen to visit a ranch and you step into a cow pie, kindly clean your boots very thoroughly before tracking bacteria in. But if you are consumer who does not live on a ranch or farm, please consider these steps:
- Buy free-range poultry. Birds that are not caged also are exposed to fecal transmission of bacteria but fewer birds are exposed to any one infection.
- Buy grass-fed beef. Out on the range, cows expel the bacteria in their digestive tracts and move on. On a feedlot, they are infected over and over again.
- Cook eggs, poultry, beef, and pork thoroughly. Pink is OK. Bloody is not.
In parts of Europe, fertilizing fields with animal manures is a health concern. In the United States this is almost never done, except by home gardeners. If you use manures in your home garden, make sure they are thoroughly composted. Compost should not smell or look like the manures from which it is made. Don't open the bag if it smells.
If you eat meat, encourage healthy and sustainable production practices by buying locally when you can, preferably directly from the farmer and buying organic, grass-fed, and free-range products. Or even better, find plant proteins you enjoy.
- Tom Levitt, "Overuse of drugs in animal farming linked to growing antibiotic-resistance in humans," The Ecologist, 23 May 2011.
- Photo courtesy of jkgroove on Flickr: www.flickr.com/photos/jkgroove/2218094907/

