A patient dealing with multiple sclerosis suffers a great many challenges, not the least of which is mobility. With the nervous system under attack and progressively worsening, symptoms can be hard to tolerate, and it’s important to keep a positive attitude as well as to seek out the proper treatments and therapies to help manage the disease, since there is no cure.
In fact, this is true of many neurodegenerative diseases, including Parkinson’s disease. Both conditions can greatly affect quality of life, and both need to be identified early in order to treat in a way that could reduce symptoms and slow the advancement of the disease. In fact, Parkinson’s and MS are similar in a number of ways. However, treatment options are quite different, so it’s important to distinguish the two separately.
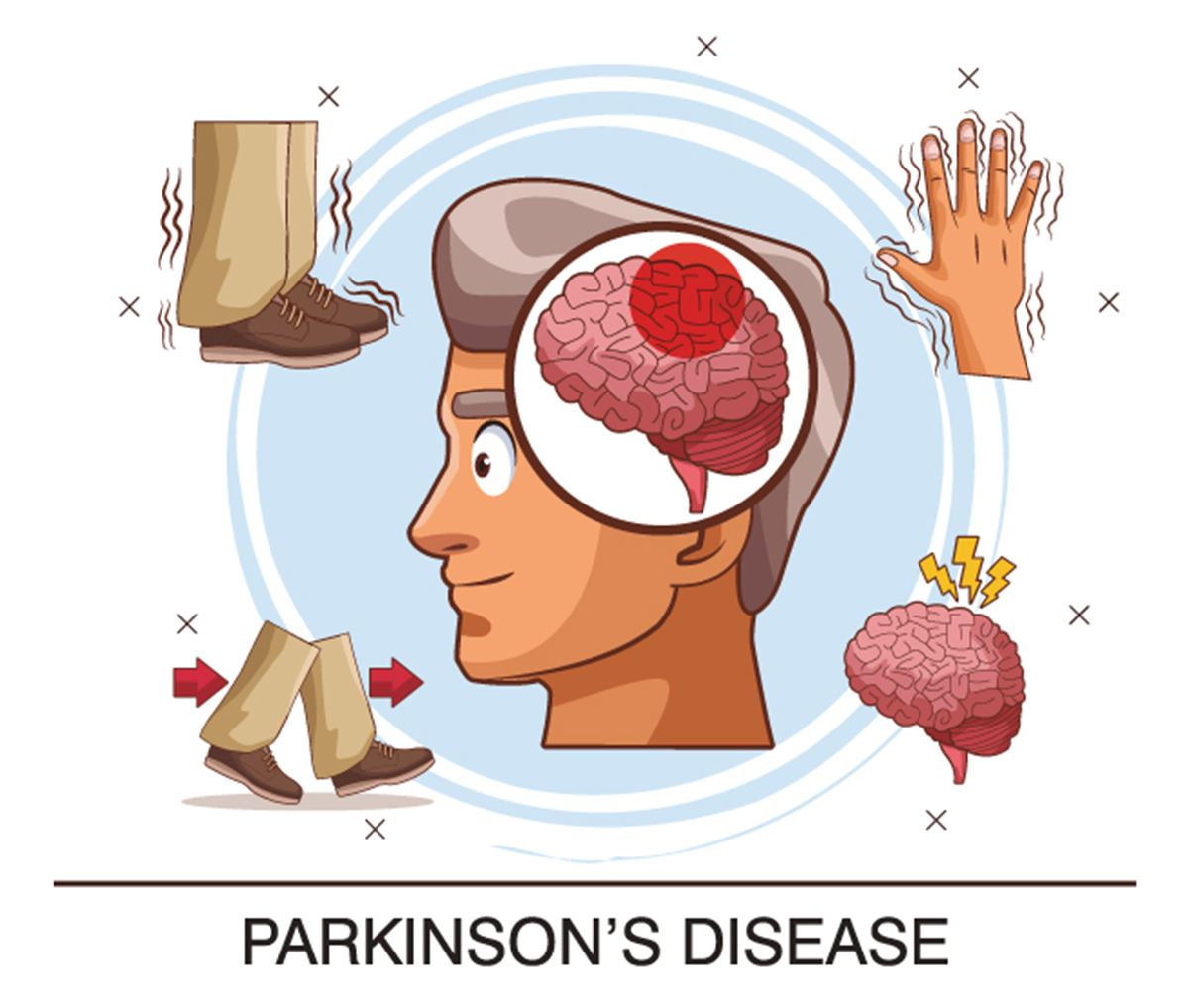
What is Parkinson's disease?
Parkinson’s disease affects the nervous system, with progressive damage. It affects the patient’s movements in a number of ways, with symptoms coming on gradually so that the patient may not even notice them at first. While the exact cause of Parkinson’s disease is not known, the action that occurs to create the problem is. The neurons in the brain begin to break down, and since neurons produce dopamine, this leads to a significant reduction of the chemical in the brain. Dopamine regulates brain activity, and when it is in low supply, patients experience abnormal activity, which leads to the symptoms of Parkinson’s.
In most cases, Parkinson’s is diagnosed in later life, with most patients over the age of sixty. Heredity doesn’t play a major role, but if a patient has several family members with the disease, the risk is increased. The same is true of exposure to certain toxins, such as pesticides over long periods. Men are also at greater risk of developing Parkinson’s than women.
Parkinson's disease and multiple sclerosis: symptoms and similarities
Since both diseases are part of the central nervous system (CNS), it’s no surprise that many of the symptoms, especially initially, are the same across multiple sclerosis and Parkinson’s. And since neither of them follow a particular pattern, creating a unique experience for every patient, it also makes sense that neither has a cure.
Some other similarities include:
- Trembling fingers, hands, and lips
- Numbness and/or weakness in the limbs, especially in the legs
- Unsteady gait, often with stiffness or rigidness
- Difficulty controlling muscles, usually symptomatic on one side before affecting the other
- Spasms in the legs or arms that are uncontrollable
- Difficulty with balance and/or dizziness
- Impaired or slurred speech, or difficulty chewing and swallowing
- Issues with bladder and bowel control
- Increased symptoms of depression
- Fatigue, generally as well as brought on by sleep problems
- Problems with vision
- Pain, especially in the limbs but possibly anywhere in the body
- Cognitive issues and “foggy” brain
- Both diseases are progressive, with symptoms worsening gradually.
While the list of similarities is quite long, there are distinct differences that change the course of the diseases as well as setting them apart in terms of available treatments. Even the risk factors vary.
Parkinson's disease and multiple sclerosis: conditions and differences
It’s important to note that, while both Parkinson’s and multiple sclerosis are diseases of the CNS, they don’t originate in the same way. MS is an autoimmune disease, brought on by the immune system attacking myelin, the protective coating over the nerves in the CNS that also speeds up signals. This affects mainly the brain and spinal cord, though it can also affect the optic nerve as well. In Parkinson’s disease, the neurons in the brain die off without any known attack, with the lack of dopamine they produce leading to the onset of the disease. This doesn’t affect nerves in the spinal cord.
Other notable differences include:
- Risk factors – Age and gender are crucial in the likelihood of the symptoms being related to one of these diseases. In MS, women are three times as likely as men to develop the disease, and the vast majority of patients diagnosed are adults under the age of fifty. On the other hand, Parkinson’s is a greater threat for men, and while it can be diagnosed at any age (just like MS), most patients are over the age of sixty.
- Treatments – MS patients typically receive corticosteroids during flare ups to control inflammation, as well as continuous treatments like beta interferon (anti-inflammatory), and other DMTs (disease modifying therapies) such as immunosuppressants or even plasma exchange. With Parkinson’s, the regimen is different, with treatments that include anticholinergic drugs (for tremors), medicines that boost dopamine levels, and deep-brain stimulation with electrodes.
- Presentation – While both diseases are progressive, the symptoms of Parkinson’s are typically so mild at first the patient doesn’t recognize them. In addition, the symptoms, once identified, are constant and progressive, worsening over time. In multiple sclerosis, the initial presentation of symptoms is typically notable. However, for most patients, they will last one or a few days before going into remission and reappearing again a month or more later. This repetition may advance into the full on secondary progressive form of the disease later, but during relapsing-remitting MS, there is rarely a notable worsening of symptoms.
- Diagnosis – In order to diagnose MS, a patient must go through a battery of tests that both suggests MS and negates any other potential cause of the symptoms experienced. This takes time and patience on both the part of the patient and the physician. With Parkinson’s there is no specific test to run. The neurologist will determine a diagnosis with a patient history, a physical exam, and a neurological exam.
Conclusion
When neurodegenerative diseases come into play, having a level head and getting a clear diagnosis is crucial to learning to cope with the diagnosis. There may not be a cure for everything, such as is the case with Parkinson’s disease and multiple sclerosis, there are plenty of treatments and ways to improve the overall quality of life, as well as the prognosis for the future. And since these two conditions that have similar symptoms, it can be easy to confuse them, especially since they can cross over the age gap despite typical age of diagnosis. Consulting a professional who can tell the difference can help a patient move forward with therapy and treatment sooner for a better outlook on the future.


Your thoughts on this