Once thought to be much rarer, multiple sclerosis has come into play as a more common neurodegenerative disease than physicians and researchers thought only a year ago. With nearly one million cases thought to plague the population of the United States alone, that’s almost two and a half times as many as were estimated a short time ago. That makes it a priority among diseases that has yet to be cured.
Luckily, Schilder’s disease is far less common. This extremely rare disease also has no cure and appears with very similar symptoms to multiple sclerosis. Also known as diffuse cerebral sclerosis and myelinoclastic diffuse sclerosis, this is another neurodegenerative disease that affects the myelin coating that protects the nerves in the CNS (central nervous system). While the name sometimes has it confused with Addison- Schilder, also known as adrenoleukodystrophy, the two diseases are not the same.
What is Schilder's disease?
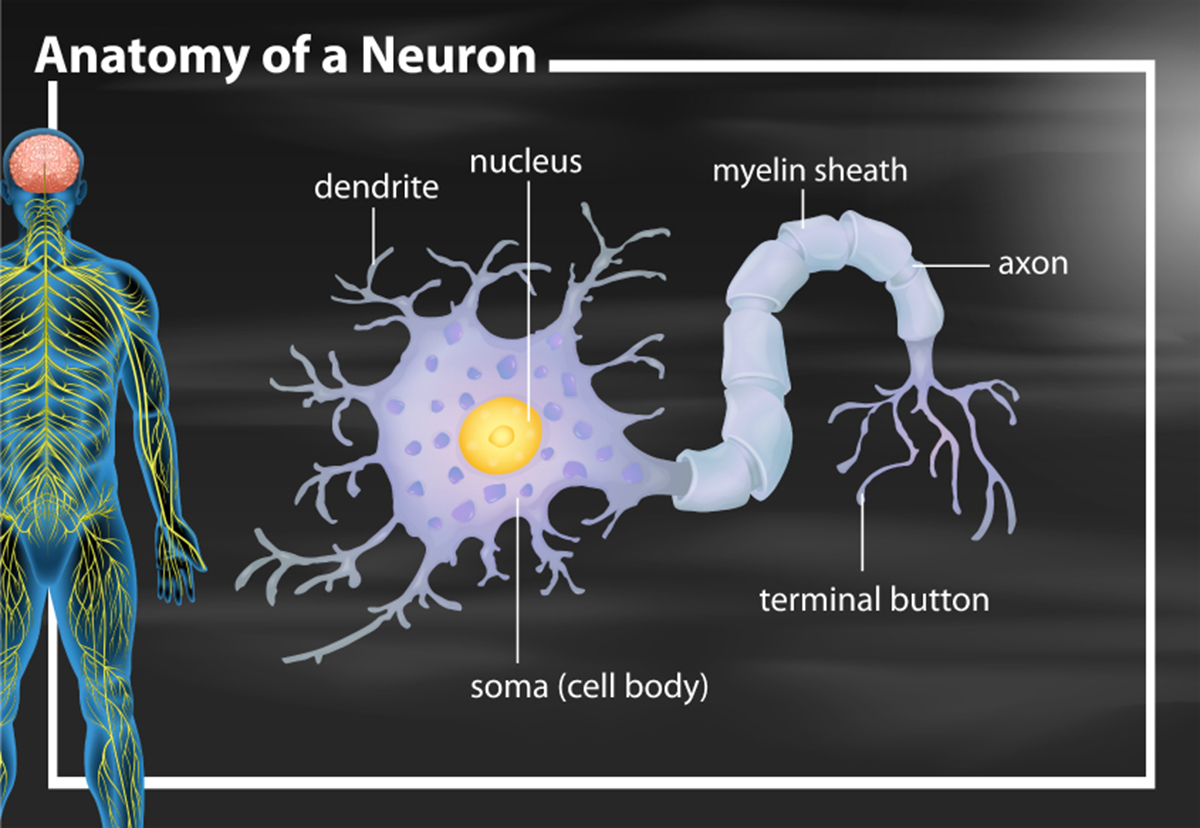
Schilder's disease is a disease that affects the myelin coating of the CNS. This coating not only protects the nerves from damage by external sources, such as free radicals but also assists with the proper speed and signal function of electrical impulses that run through the body between the brain and the peripheral nerves. While the exact cause of the disease isn’t known, the condition is often labeled as a form of multiple sclerosis and is defined as an autoimmune disease because the damage is caused by an attack on the myelin by the immune system.
With a very similar occurrence leading to symptoms and the belief that Schilder's disease could be a form of MS, it’s no wonder they are so much alike, especially in terms of symptoms. However, not everything is the same, which is why Schilder's disease receives a separate diagnosis.
Schilder's disease and multiple sclerosis: symptoms and similarities
With multiple sclerosis and Schilder's disease, almost all the symptoms are the same, with very few differences. Because they are both difficult to diagnose, there is a battery of tests involved in the determination of each disease, with each including a physical exam and the potential request for an MRI. Both diseases are treated with similar medications, depending on the severity and the patient’s needs, including corticosteroids to help with inflammation during flare ups, beta interferon to control inflammation constantly, immunosuppressants to calm the immune system (one of several disease modifying therapies, or DMTs, available), and both physical and occupational therapy.
Similar symptoms include:
- Muscle weakness, usually beginning on one side of the body
- Mobility issues, including slowness and stiffness
- Chronic headaches
- Hearing and vision trouble (especially blurred vision or eye pain)
- Tremors and spasms, especially in the legs or face
- Issues with balance and dizziness
- Difficulty with speech or swallowing
- Memory, attention, and cognitive issues
- Tremors and the possibility of seizures (although not as common)
- Trouble with control of bladder and bowels
Of course, while the two diseases do seem to mirror each other almost perfectly in many ways, Schilder's disease and multiple sclerosis are quite different in others, including some of the symptoms that present in Schilder's disease, as well as the demographics often involved in their appearance.
Schilder's disease and multiple sclerosis: conditions and differences
While multiple sclerosis is fairly prevalent for a neurodegenerative disease, Schilder's disease is extremely rare. In fact, some feel that no more than twenty-nine cases have ever been definitively diagnosed accurately, since so many of the symptoms are similar.
Some of the symptoms that may occur in Schilder's disease but not in a typical case of multiple sclerosis are:
- Nausea and vomiting
- Malnutrition
- Trouble with respiration, blood pressure, or heart rate
- Increased irritability
- Extreme personality changes
- Less awareness and unresponsiveness (over time)
While there are no specific diagnostic tools for either disease, the regimen of testing is different for each. In multiple sclerosis, physicians usually order an MRI, a spinal tap, and an EP (evoked potential) test. To diagnose Schilder's disease, doctors may ask for an MRI and perform an EEG. In addition, there are some conditions to meet to confirm the diagnosis:
- The patient has one or two lesions of at least 2cm diameter that are close to symmetrical on the brain.
- These are the only lesions found anywhere in the central nervous system, and there is no evidence of compromise to the peripheral nerves.
- Tests of the adrenal system prove normal, ruling out adrenal related diseases.
The risk factors for Schilder's disease and multiple sclerosis are extremely different from each other. In the case of MS, the average patient is between eighteen and forty, though various types may have different age ranges, and it can be diagnosed at any time (though very rare in children and older adults). For Schilder's disease, the symptoms usually begin in childhood, with a typical diagnosis between the ages of seven and twelve, though again, this is not the only age for symptoms to appear. Also, women are three times as likely as men to develop MS, whereas Schilder's disease is more common in males.
With Schilder's disease, there are large patches of myelin missing, and lesions occur only in the brain. In MS, the myelin could be damaged in large patches or in small, microscopic amounts spread out through the CNS. Lesions can occur in the brain, on the spinal column, or in the optic nerve. While both diseases are unpredictable in their progression and the path they take, MS is not fatal, with patients often living a normal lifespan. This can be the case in Schilder's disease, but it can also be fatal in some cases.
Conclusion
If someone is experiencing symptoms that relate to multiple sclerosis or Schilder's disease, it’s important they consult with a physician as soon as possible. Starting the process of diagnosis is essential to a good prognosis and a promising future. Neither disease has a cure. However, there are lots of treatment options to reduce symptoms and slow the progression of the conditions, allowing greater independence and less suffering, as well as fewer flare ups of symptoms. The sooner someone goes through the testing process, the sooner they can start managing their symptoms.

