Loading...
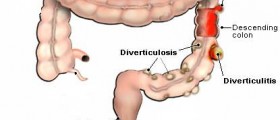
Treatment for diverticulitis focuses on clearing up the infection and inflammation, resting the colon, and may prevent or minimize complications. If you are suffering from acute diverticulitis, you should consult your doctor prior to taking anything.
An acute attack with severe pain or severe infection may require a hospital stay. Most acute cases of diverticulitis are treated with antibiotics and a liquid diet. The antibiotics are given by injection into a vein. In some cases, however, surgery may be necessary.
When is surgery necessary?
If attacks are severe or frequent, your doctor may advise surgery. The surgeon removes the affected part of the colon and joins the remaining sections. This type of surgery, called colon resection, aims to keep attacks from coming back and to prevent complications. The doctor may also recommend surgery for complications of a fistula or intestinal obstruction.
If antibiotics do not correct an attack, emergency surgery may be required. Other reasons for emergency surgery include a large abscess, perforation, peritonitis, or continued bleeding.
Emergency surgery usually involves two operations. The first surgery will clear the infected abdominal cavity and remove part of the colon. Because of infection and sometimes obstruction, it is not safe to rejoin the colon during the first operation. Instead, the surgeon creates a temporary hole, or stoma, in the abdomen. The end of the colon is connected to the hole, a procedure called a colostomy, to allow normal eating and bowel movements. The stool goes into a bag attached to the opening in the abdomen. In the second operation, the surgeon rejoins the ends of the colon.
Loading...
Loading...
I'm 24. I recently had an op to remove a large benign cyst from my abdomen. Everything went well until a few days later when my bowel perforated and I developed faecal peritonitis. I too had the NG tubes, inserted several times whilst awake, which stayed in for a week or so. However whilst in excrutiating pain for 3 days I was on NO intravenous pain relief, but instead was given tablets, which could be seen travelling up the tube into the bile bag as soon as I took them.
My symptoms were ignored by the medical staff, who didn't seem to believe I was in pain. Eventually after several days of steady deterioration my surgeon showed up and I was whipped into surgery. From the onset of symptoms of the peritonitis to the surgery was about 40 hours.
Because of the delay in diagnosing my condition I've been absent from work for 5 months now. I'm starting a phased return to work (I'm an accountant) this week.
However I'm hoping to have my loop colostomy reversed as soon as possible because it seems to be getting bigger and is getting harder and harder to conceal.
I've got this operation to go, and then corrective cosmetic surgery to restore some degree of normality to my abdomen. How long should I expect the recovery period from the reversal operation to be?
Loading...
Thanks, khbme2u.
Loading...
It is April 8th 2011. I am scheduled for a colostomy reversal in May. Would like to hear more abour your experiences. Will write about mine when I am certain you guys are still writing and I am not the only one SMILE.
Best to all!
Susan
Loading...
HI, I am 34yrs old and was diagnosed with Diverticulis last yr, May 2010.. I was scheduled to have the colon resectipn surgery laporascopic but 2weeks before the surgery I had an attack, went into the hospital and while I was admitted my colon preforated and I had to have an emergency colostomy. I was so afraid and dreaded having it done especially because I did not want a colostomy bag. I was depressed the 1st 2weeks, but with the support of my family and friends I was able to get out of that depression and realize that I was lucky to be alive and that there are so many other people out there that are going through worse situations and that my situation is temporary. I took some sick leave off from work hoping that durring that time I would have it reversed but unfortunately my surgeon wanted to wait a full 3months recovery before he did the reversal since he wants to do it laparoscopic. I am scheduled to have the reversal in 4days on Monday 4/25/11. I am scared of going under but at the same time so looking forward to getting rid of this colostomy bag. This being my last week, it has been irritating me and not cooperating, having to change it every 2days and my skin is getting so irritating and raw. I have appreciated reading so many of your stories. When you go thru something like this sometimes you feel alone and that noone around you understand you or what your going thru. I am glad I am able to read what to expect after my reversal, and I see that I have to truly watch what I eat. I hope everyone is well and recovered and God Bless you all.
Loading...
Loading...
Loading...
After over 2 weeks of suffering and loosing strength and massive weight loss while trying to maintain my security job, I finally went to a hospital and discovered I had ruptured and would require surgery.
The doctor had hopes of using a drain to reduce intestinal swelling and be able to remove the damaged section avoiding the necessity of a colostomy.
When I went to surgery I didn't know if I would have a colostomy or not (I did).
Something went wrong with the first procedure and they had to go back in a second time a few days later.. If I read it right in the medical records at some time during the second surgery I had to be revived..
They had planned to do a reversal a few months later but I ended up fighting massive infection in the incision which put me in and out of the hospital, the installation of a wound vac and a month in a nursing home .
In all I spent 7 months with a colostomy
( Free tip - Don't eat Lee's famous recipe if you have trouble with the bag detaching in the middle of the night. The other nursing home residents won't appreciate "gassing" 1/2 the building)
It's been 4 years since the reversal (Valentines day of all days no kidding) .I have never fully recovered my strength and stamina from my body feeding on itself and the long stays in the hospital and nursing home.
When I tried to go back to the security company I worked for the past 9 years (even though still weak) they claimed that their old office staff said that I had quit.
( 3 months before I was released by the doctors while on emergency medical leave? Yeah, Right! give me a break).
With 2 disabling injuries from work (12% permanently disabled according to workman's comp) along with my weakened state at the time, my wife tried to help me get on disability. Even though they (SSDI) agreed that I had multiple problems, They said that none of them were severe enough to qualify.
So Now I'm sitting here no insurance, jobless, living barely on my wifes income, eyesight going bad from untreated diabetes, In pain 1/2 the time either from work injuries or from the after effects from the last surgery. Small herniation's along the incision along with problems from the plastic sutures they used. pain from the titanium staples they use to staple your intestines back together.....
Sometimes the doctors go too far without regards to quality of life.
Loading...
I was involved in a near-fatal motor vehicle accident on March 3, 2011. The seatbelt mangled my small bowel and as a result I received a temporary colostomy. I am scheduled for my reversal October 4, 2011 and I cannot wait. Having this bag attached to my side has been horrible, but like everyone says, "at least I'm alive".
I too had the awful leaks, the painful skin irritations and rawness, the feeling of being dirty all the time, etc.
I found this site because I wanted to know what to expect after my reversal surgery. I sometimes feel my surgeon isn't as forthcoming with information as he could be. I gained some extremely valuable information, got most of my questions answered, and don't feel quite as bad now. Thank you to everyone!!
Loading...
The worst part of the reversal for me (done 10/5/11) was gas pain. It can be pretty bad, but getting up and walking really helped to get it out. The surgery itself went really well, it took 1 and 1/2 hours, and I was able to go home after I got some of the gas out of me (home today Oct 8th).
I made sure that I went to a colorectal surgeon, not a general surgeon. That may make all the difference in outcome. My temp colostomy was done by a general surgeon in an emergency situation. I lived for 2 months with a 4" prolapsed stoma--talk about hard to live with. I couldn't even go to work! This time around the incision was neat, and I can tell it will heal nicely.
There's going to be some bloating in the abdomen for awhile, and the gas will come and go. Overall, I'm really comfortable and weaning off the pain meds. You just have to take it easy for several weeks. Overall the reversal was totally worth it. Hope yours went well.
Loading...
Nov 25, 2011.. hello all had my reversal colostomy done on Nov 15th took 5 days to pass gas after which I had some complications but then got back on track. Starting have some solids on Nov 23rd and since starting to pass gas with a very small amount of leftover I call mucus in my bowel movement I have yet to have a real stool BM, just wondering what others timeline was for passing there first real BM after starting to eat solids. I'm not looking for my stool to be solid, I know this will take time but even running stool? thanks in advance, curious in Toronto
Loading...
Loading...
Loading...