Over 604,000 women will be diagnosed with cervical cancer every year across the globe — and 342,000 of them will die from the disease. Despite the fact that any woman, anywhere, can develop cervical cancer (the US sees around 13,000 new cases and 4,000 deaths annually, for example), this cancer disproportionately kills women in low and middle income countries. That is, 90 percent of cases and deaths occur in poorer regions.
The good news? Modern medicine already has all the right tools to stop cervical cancer, or at least make it exceedingly rare. The challenge lies in implementing those tools across the world.
Do you live in a place where you have access to modern medical care? Do you have a cervix? Have you not been screened for cervical cancer in a while? Now's the time to check whether it's time to attend a simple and potentially life-saving screening procedure.
What Is Cervical Cancer?
A 2020 UK survey revealed that half of British women don't know where their cervix is. It's not strange to think the situation is likely to be similar in other countries, or that many women don't know what the cervix does, either. Let's start with that.
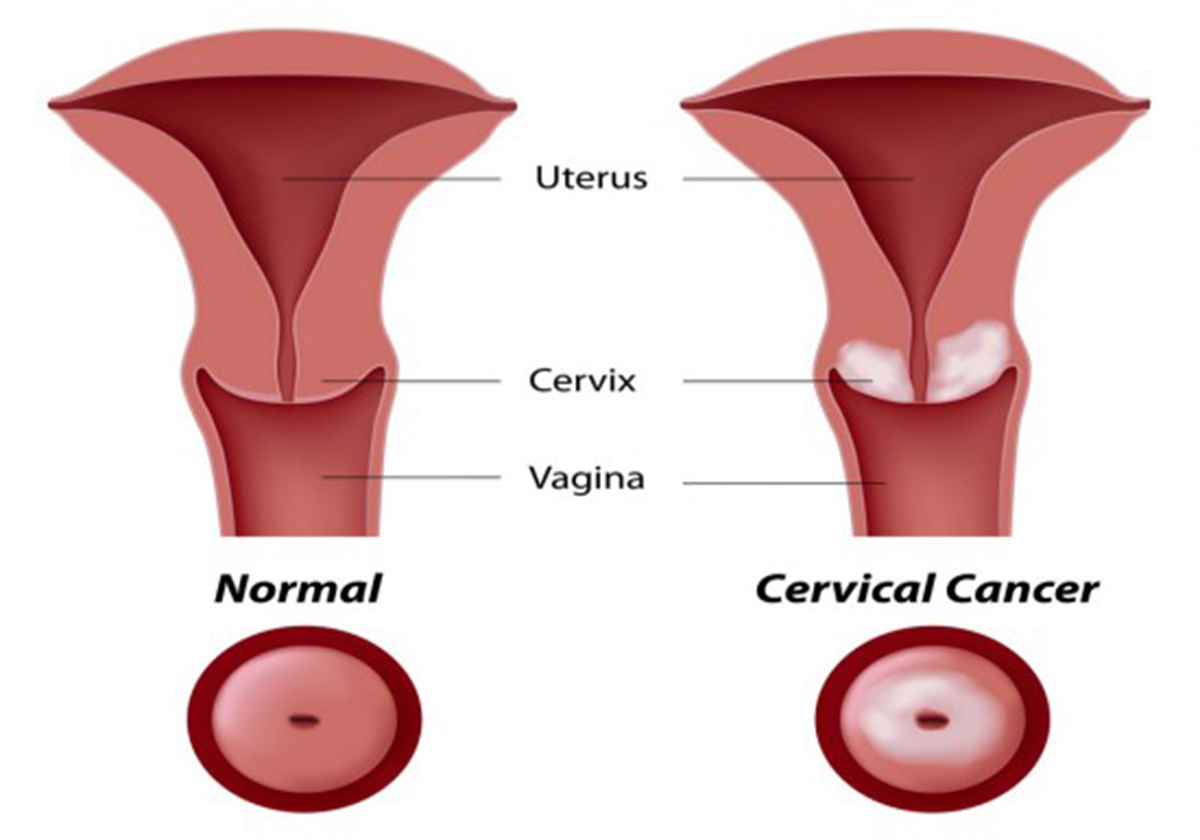
The cervix is the lower end of the uterus (womb). It is a narrow opening that connects to the vaginal canal. This is the part of the body doctors refer to when they say a woman in labor is "10 centimeters dilated" — because the cervix has the ability to open up to let a baby through. It also changes position as the menstrual cycle progresses, and allows the menstrual flow to come out.
The cervix is composed of two main parts. The ectocervix, the outer part, can be seen during a medical exam. Women can also locate their own cervix by inserting their fingers. The inner part, the endocervix, produces mucus and links up with the uterus.
Cervical cancer is cancer that starts in the cervix. There are two main types:
- Squamous cell carcinoma is most common and develops in the ectocervix.
- Adenocarcinoma develops in the endocervix.
Learn more about cervical cancer causes, symptoms, and treatment by clicking on the link!
Here's the thing. The overwhelming majority of cervical cancer cases — 95 percent! — are caused by the Human Papilloma Virus (HPV). This sexually-transmitted infection is so common that most sexually-active adults develop it at some point. Many cases subside, but others become chronic. It can then take 15 to 20 years for cervical cancer to develop.
That's a long time — and we already have tools to prevent the body from making that potentially-deadly leap.
Cervical Cancer Prevention: What Tools Are Available?
Not all of the over 100 types of HPV cause cervical cancer, or even effect the genital area. We already have some powerful tools to reduce the risk of being exposed to the ones that do (mainly types 16 and 18), and to slash the odds that a HPV infection becomes cervical cancer:
- Condom use doesn't prevent a HPV infection entirely, but it helps.
- Not smoking is another way to reduce your risk of cervical cancer, as smoking raises the risk of developing cancer significantly.
- Not having sex with multiple partners and at a young age is another way to reduce your risk of developing cervical cancer.
- Not using oral contraceptives long-term also reduces your risk of cervical cancer.
Medically, we have two main ways to reduce the risk of cervical cancer. They are:
- The HPV vaccine. The HPV vaccine has been shown to be a safe and effective way to prevent cervical cancer over the course of 15 years. It is routinely offered to young people aged 11 to 12 in many countries now. You can still get it if you're older, especially up to 26.
- Pap smears. Pap smears or Pap tests are performed at the doctor's office. The practitioner inserts a speculum and takes a swab of cervical cells to detect cells that may become cancerous if left untreated. The test is recommended once every three years for women aged 21 to 65.
- HPV tests. A HPV test detects whether you have HPV, including the typs of HPV associated with cervical cancer. The test is usually done at the same time as a Pap smear. The procedure is the same, although once the swab is sent to the lab, technicians look at different data.
If a Pap test shows abnormal cells (pre-cancerous cells that may develop into cervical cancer in the future), your doctor may recommend a colposcopy to get a closer look. A minor surgical procedure can be performed to excise the abnormal cells. This is called a LEEP procedure. Cryotherapy and laser therapy are also available. If your HPV test comes back positive, watchful waiting is recommended to see if the HPV clears on its own.
Getting tested for HPV and undergoing a Pap smear may be scary if you think there's a good chance you've been exposed. Remember that timely treatment is your best chance of a good outcome, even if you do have a type of HPV associated with cervical cancer. If you didn't benefit from a HPV vaccine, cervical cancer screening is your most powerful way to prevent cervical cancer.


Your thoughts on this