Effects of autoimmune diseases
Autoimmune conditions have one of three characteristic pathological effects which allows the conditions to be classified as autoimmune issues. They are:
- Damage or destruction of the affected tissues.
- Modified organ function.
- Changed organ growth.
Symptoms
It's important to remember that autoimmune conditions can affect many parts of the body. This means that symptoms can be non-specific and generalized in nature. The symptoms could include fever, fatigue and a general feeling of being unwell (malaise). These symptoms tend to improve during remission phases and get worse during flare-up episodes.
How is the diagnosis made?
A complete and accurate history, a physical examination of the patient and a high index of suspicion will point the doctor in the right direction regarding appropriate tests that need to be done.
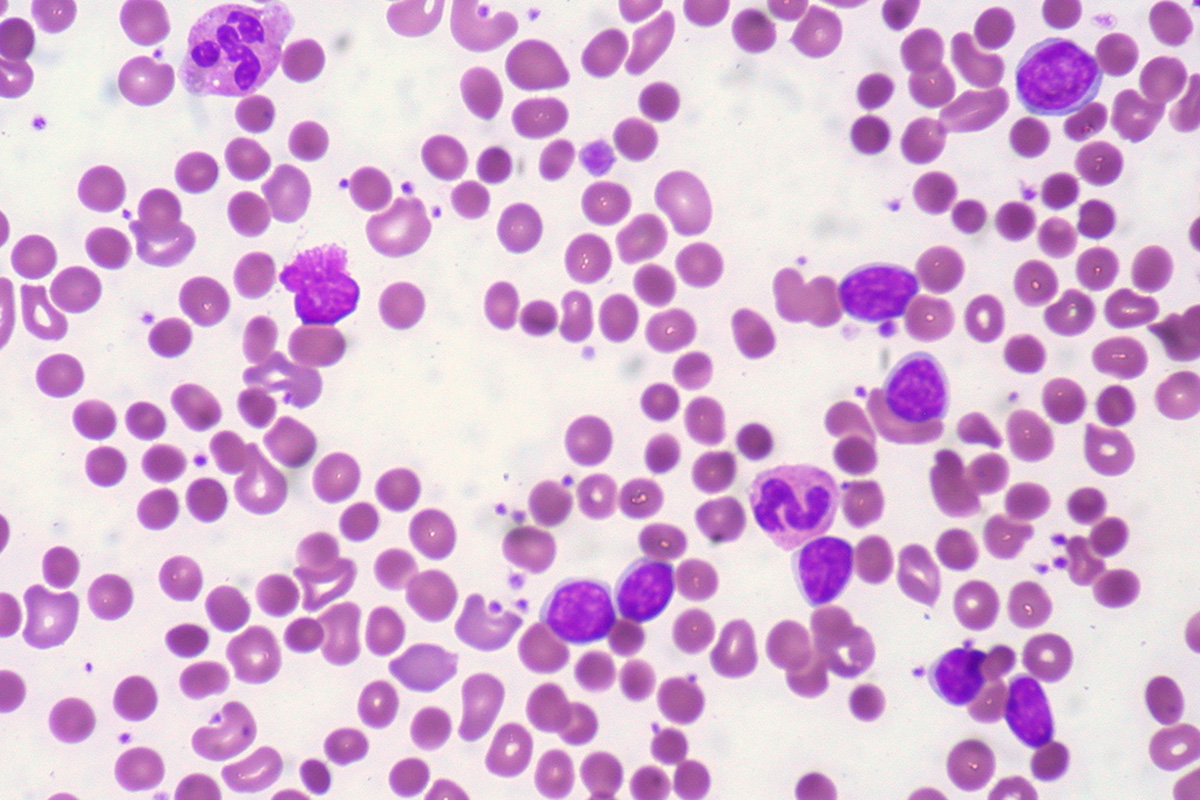
Blood tests which could point to autoimmune conditions include inflammatory markers such as elevated white cell counts on a full blood count (FBC), an elevated C-reactive protein (CRP) and an elevated erythrocyte sedimentation rate (ESR). Other serological tests, such as auto-antibody tests, can also be requested depending on the signs and symptoms the patient is presenting with.
Ultrasounds, CT scans and X-rays can be done to investigate organs, tissue and bones which may be involved in the suspected autoimmune disorder.
Preventative measures
There are some measures which can be taken by the affected individual to regulate their immune system in order to reduce symptoms of autoimmune conditions.
These measures can include the following:
- Omega-3 fatty acid supplementation - Omega-3 fatty acids counteract the effects or arachidonic acids which aggravate symptoms of autoimmune conditions. This fatty acid is included in the treatment protocols of issues such as rheumatoid arthritis, asthma, inflammatory bowel disease and psoriasis. Omega-3 is also used to decrease the physiological symptoms of depression as they are autoimmune and inflammatory in nature.
- Sunlight/conversion of vitamin D - adequate levels of vitamin D in the body allow for a better functioning immune system. This is due to the fact that T and B immune cells include receptors for vitamin D to bond to them.
- Probiotics - Bacteria such as Lactobacillus casei have shown to stimulate the immune response against tumours and also regulate immune function. This has resulted in the prevention of type 1 diabetes mellitus.
- Antioxidants - It's been hypothesized that type 1 diabetes is as a result of free radical formation. It has been thought then that a high intake of antioxidant supplement by pregnant mothers could counter this effect.
READ Antioxidants-Your Defense Against Free Radicals
- Reduce stress - Emotional and physical stressors can cause the release of cortisol and catecholamines which negatively impact the immune system. This would then result in an increased risk of flare-ups. Regular exercise and relaxation techniques would be very beneficial in this regard.
Common Autoimmune Diseases And Their Specific Management Protocols
Type 1 diabetes mellitus
Type 1 diabetes occurs due to antibodies attacking the insulin producing islet cells of the pancreas. The pancreas therefore can’t produce insulin anymore and the body’s glucose levels can’t be controlled.
Management of this condition then involves external administration of insulin on a daily basis and having to maintain strict dietary guidelines and stay physically active.
Rheumatoid arthritis
This condition occurs when the joint spaces and the surrounding tissue are attacked by antibodies leading to increased inflammation of the joints. The fingers, hands and wrists are usually the most involved areas. This can lead to decreased mobility and increased deformity of these areas.
Management includes using medications such as non-steroidal anti-inflammatory drugs. For more severe cases medications such as those that reduce cell growth, corticosteroids and certain anti-malarial drugs are also used to try and reduce the inflammation caused by this condition.
Systemic lupus erythematosus/Lupus (SLE)
Lupus is a condition where nearly every area of the body had been attacked by antibodies. The areas involved include the skin, joints, brain, kidneys, heart, liver and lungs.
The way to manage this condition is to control the flare ups of inflammation in the mentioned areas. This is done by using drugs such as corticosteroids and cyclophosphamide.
Vitiligo
The antibodies here attack the pigment cells of the skin thereby causing patches of decreased pigmentation. These white patchy areas can be mild or quite pronounced and can involve any part of the skin. The biggest issue with vitiligo is the cosmetic effect it has especially if it involves younger patients.
The management of this issue involves using make-up and cosmetics to cover the white patches especially if the face is involved. Phototherapy and using immune suppressing creams are also part of the management of vitiligo.
Psoriasis
Antibodies attack the skin and can cause inflammation in the affected areas. These areas become red and irritated and then go on to become thickened, flaky and with silver-white patches. The most commonly involved areas include the scalp, back of the forearms, around the belly-button and the shins.
Drugs such as vitamin D analog creams, topical steroid creams and emollients were found to be useful in reducing the effect of this condition.
Grave’s disease
The thyroid gland is attacked by antibodies here which cause inflammation of the organ. This then leads to swelling of the thyroid and it becoming overactive. Other characteristic signs of this disease include bulging eyes.
Compared to other autoimmune conditions, Grave’s disease can actually be treated. Anti-thyroid drugs can be used for mild cases but more severe cases may need radioactive iodine or surgical removal of the thyroid.
Inflammatory bowel diseases
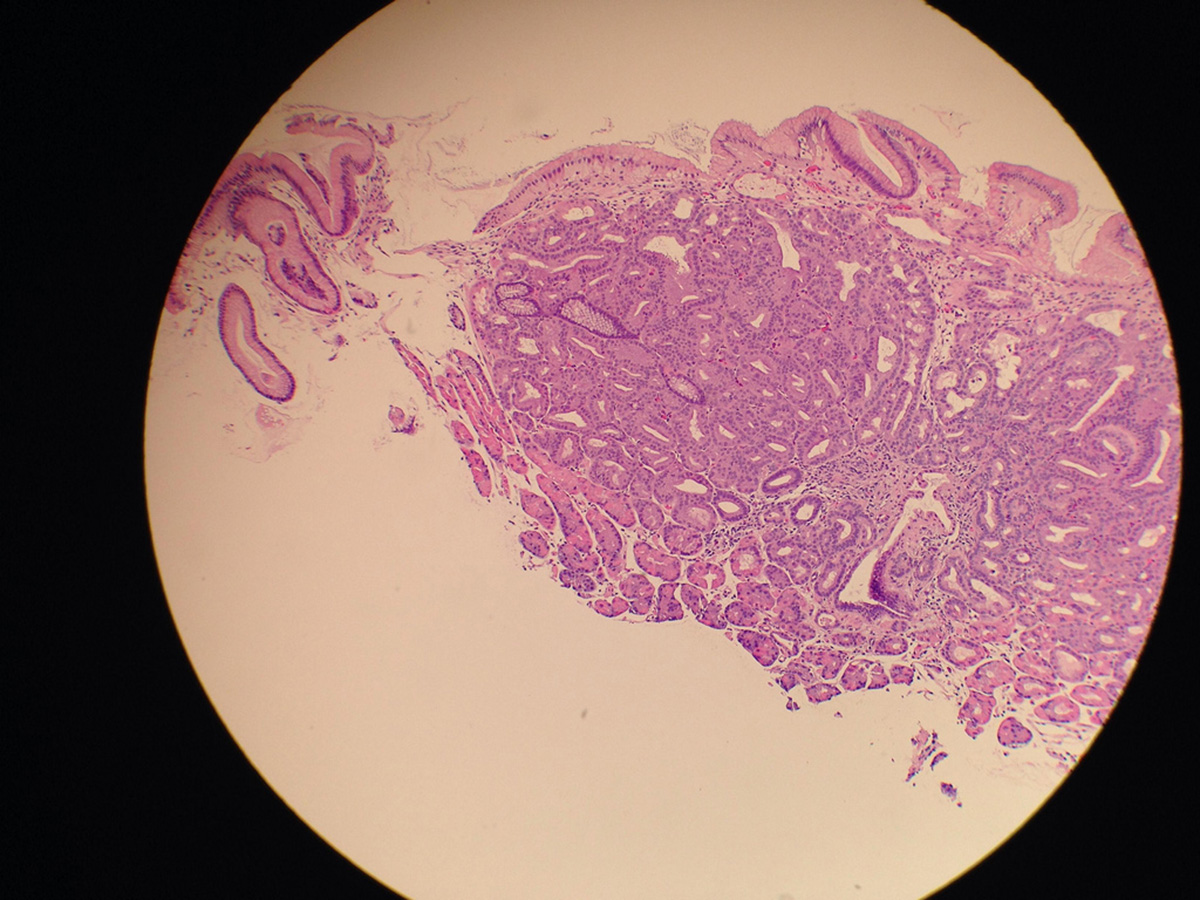
The small and large intestine can be involved here and include conditions such as Crohn’s disease (can involve the mouth up to the anus) and ulcerative colitis (involves the colon and rectum only).
Crohn’s disease can be managed over the long-term with antibiotic use. Ulcerative colitis can be managed with drugs such as meselazine but surgical removal of the affected area is more curative.
READ Lupus in Women: Chronic Inflammatory Disease
Celiac disease
This condition is caused by a reaction to gluten (which is contained in wheat, rye and barley) which results in damage to the lining of the small intestine. This can lead to absorption difficulties and long-term complications such as failure to thrive.
Dietary changes need to be incorporated where gluten has to be removed. If these changes don’t work, then steroids and immune-suppressant medications need to be used.
- www.healthline.com/health/autoimmune-disorders
- Photo courtesy of euthman: www.flickr.com/photos/euthman/3953390018/
- Photo courtesy of niels_olson: www.flickr.com/photos/niels_olson/10603315934/
- Photo courtesy of euthman: www.flickr.com/photos/euthman/3953390018/

