With multiple sclerosis, both the patient waiting to be diagnosed and the doctor trying to make the diagnosis face hardship and frustration. A patient has to deal with the unknown, having a panel of symptoms that could point to one of several serious diseases, including MS, while the doctor has to adhere to stringent criteria in order to make a diagnosis.
By the time that diagnosis is made, whether it’s MS or something else, both patient and neurologist are often relieved. It allows the patient to move on with life, no longer fearing the news and, instead, putting their efforts into creating the fullest and most comfortable life possible. Several tests play a role in coming to a final conclusion, and one of the most common tests applied by doctors is a spinal tap.
Why multiple sclerosis needs an early diagnosis
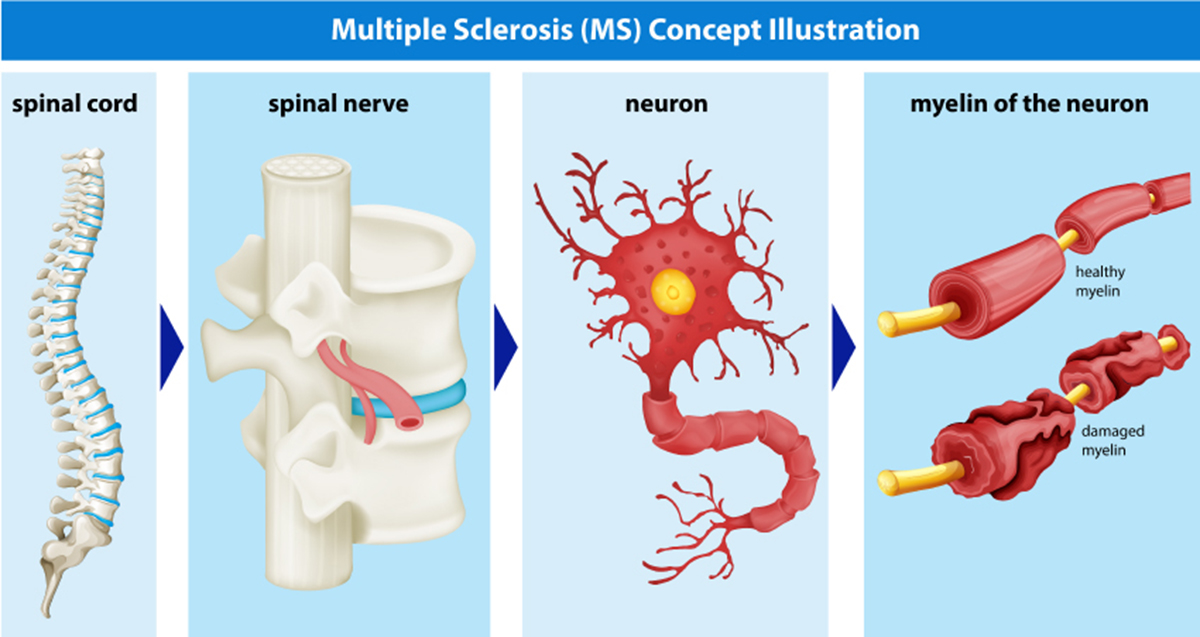
Multiple sclerosis is an autoimmune disease where the central nervous system (CNS) is attacked, causing some debilitating symptoms. Eventually, for the majority of patients, it is progressive and degenerative. The sooner the disease is diagnosed, the more treatments and therapies can be employed to change the course of the disease and help minimize damage, as well as slow progression. New information makes it even more essential to discover the presence of MS early on.
- Up until recently, doctors believed about one in every thousand people were struck with MS. However, in recent months, based on new findings, that estimate has more than doubled, meaning that the projection of 400,000 people in the U.S. thought to have MS has now increased to over a million. Higher prevalence takes higher priority.
- Also, because most patients start with a form of multiple sclerosis that “comes and goes”, doctors believed it took a long time for nerve damage to appear. However, recent studies prove that permanent nerve damage can occur in the earliest stages of the disease, meaning earlier detection is needed to prevent such problems.
One of the best ways to find out if a patient could be suffering from MS is to perform a spinal tap.
What is a spinal tap?
In a spinal tap, also known as a lumbar puncture, fluid is taken from the spinal cord for assessment. This cerebrospinal fluid, or CSF, is evaluated, in this case, for evidence that MS exists.
It’s called a lumbar puncture sometimes because the needle used is inserted through the lower back, or lumbar region, between two of the vertebrae in the spine. That needle extends into the spinal cord, where the CSF, a fluid that is found in the brain and spinal cord, surrounds those essential parts of the central nervous system to help protect them from serious injury.
Using that needle, a sample of spinal fluid is taken. CSF can be used to diagnose a number of serious ailments and conditions, such as brain cancer, a meningitis infection, Guillain-Barre syndrome, and multiple sclerosis. When the fluid is evaluated for MS, signs of inflammation, as well as the presence of the antibodies created to attack the nerves, are assessed and used to help with diagnosis.
However, because of the stringent requirements and burden of proof placed on the physician making the diagnosis, this is not enough to make a definitive decision. Therefore, the patient is put through a rigorous round of additional testing before the diagnosis can be made.
Testing for multiple sclerosis
Perhaps it’s not quite right to reference the first act as a test, though patients may feel like they’re taking a verbal exam as they have a lengthy discussion with their physician to help assess the situation. The neurologist will likely ask a lot of questions before performing a physical exam, with some of the actions including:
- Asking about recent and previous flare ups of symptoms that could be related to multiple sclerosis, such as when they occurred, how long they lasted, how severe they were, and how long between episodes.
- Asking general and specific questions about medical and family history, with some focus on place of birth, various places of residence, travels both in the past and recently, and other information that could point to some sort of exposure to another disease that could be causing the symptoms which at first appear to be related to multiple sclerosis.
- Asking about or testing functionality of speech, mental capacity, and emotional function.
- Testing several motor skills, including balance, ability to walk with a normal gait, overall coordination, reflex functionality, overall strength, weakness in the limbs, vision issues or eye pain, and some other sensory capabilities that could all be affected by damage to the central nervous system.
When the physician completes this, if there is sufficient concern that the patient has MS, the battery of tests will be ordered, including the spinal tap.
- Evoked Potential – Using electrical impulses or other sensory images and sounds, the five senses are tested, with nervous system response monitored to see if the central nervous system is delivering those impulses properly, telling neurologists if there is damage by defining if the signals are moving quickly enough and emitting the proper responses. This procedure is noninvasive.
- MRI – Magnetic resonance imagining is a noninvasive procedure that utilizes magnets to create an image of the spine and brain so that doctors can evaluate the appearance of the nerves and tissue in search of damage to the CNS, potentially caused by an attack of the immune system.
- OCT – this is another noninvasive way to help prove nerve damage by MS, since the tomography of the retina is different in MS patients than in other patients. An optical coherence tomography picks up on damage to the retinal structure and optic nerves, mainly looking for optic neuritis.
How criteria is used for diagnosis
The reason so many tests have to be run is to assure that the criteria required to be met for a diagnosis is found. Because there are a number of conditions with a very similar resume of symptoms, doctors have to be absolutely certain that the disease causing the problems is actually MS so it can be treated accordingly.
A positive diagnosis requires all of the following findings:
- The CNS (central nervous system) including the brain, optic nerves, and spinal cord, must show absolute evidence of damage in at least two separate areas;
- The damage found must be proven to have occurred in two completely separate events, or attacks to the CNS (should this not be the case, the patient may still find themselves diagnosed with the clinically isolated syndrome, which could later be upgraded to MS, if a second episode with further damage occurs); and
- That all other potential diseases and conditions which could lead to the same symptoms and damage have been ruled out as a possibility.
Initially finding the actual damage is a difficult task, but to rule out everything else that could be causing the problems is a long and grueling process. A spinal tap that shows a presence of antibodies related to a nerve attack could go a long way in showing that the damage is due to the presence of MS.
Conclusion
With so many tests to run, a diagnosis of multiple sclerosis obviously won’t happen overnight and could take some time. This can lead to anxiety and mood swings, but staying focused and finding the answer is essential to the future for any patient. The use of a lumbar puncture to test spinal fluid can go a long way in speeding up the process for both the doctor and the patient, getting answers sooner.

