With dental health, the focus is usually on teeth and often attention to the gums and other supporting structures can often be forgotten. Unfortunately, this is problematic as the whole system needs to be considered together; indeed gum health is also indicative of general health and well-being. While sore, sensitive, swollen or bleeding gums may indeed indicate early gum disease, they may also be due to other underlying issues. Regardless, you can do a number of things to manage discomfort and minimize damage to your gums which this article will set out to explore.
What is the connection between red, sore and bleeding gums and periodontal disease?
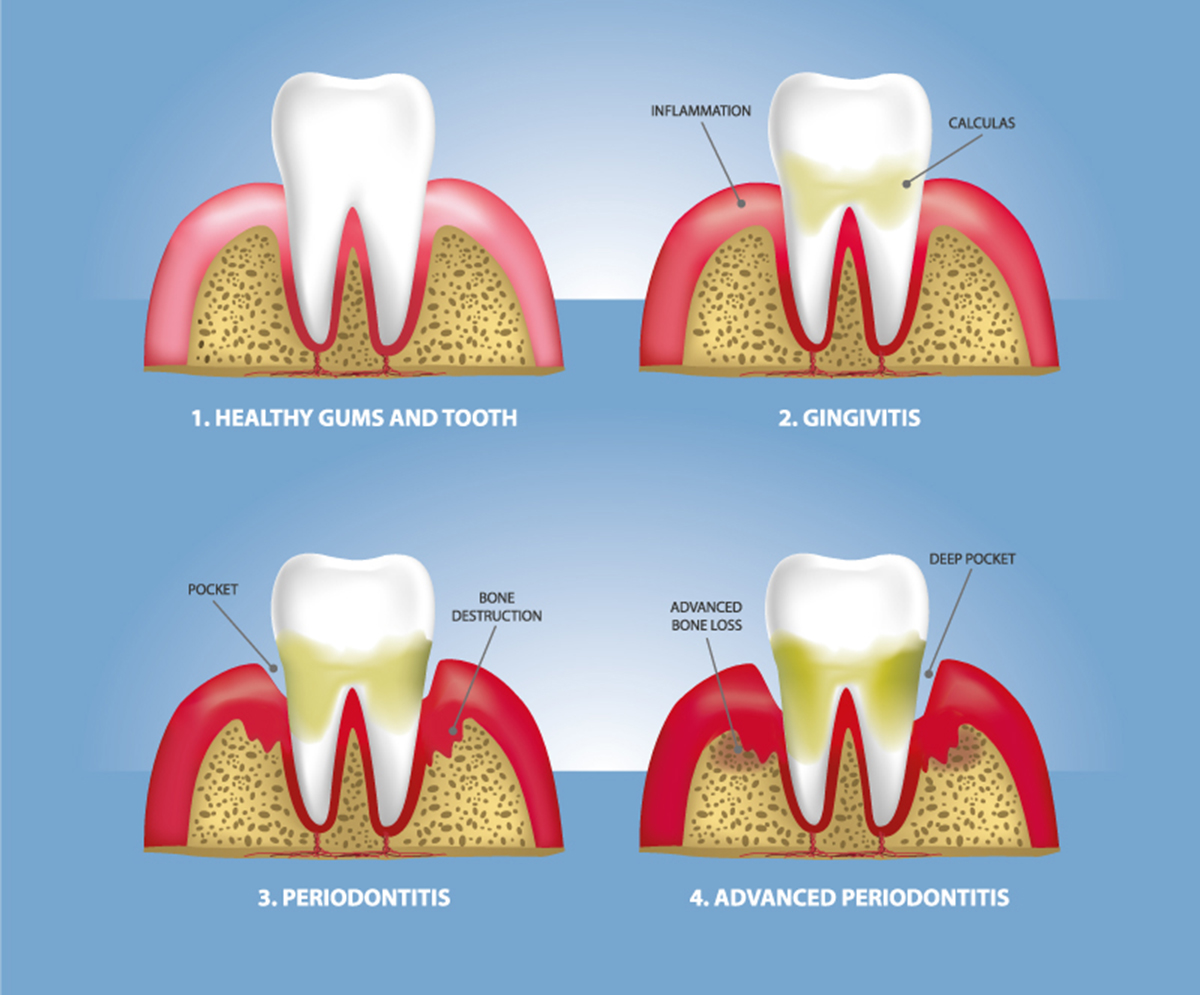
The process begins with bacteria building up on your teeth which, over time, causes layers of plaque and tartar to develop. This is known as gingivitis or gum disease. For most it causes no discomfort and may just result in some bleeding or swelling which can easily be addressed and the disease stopped in its tracks. However, if left unchecked, the disease worsens and your gums recede, creating pockets that can become infected. The bone and tissue in your jaw that hold your teeth in place then deteriorate, and eventually your teeth may become loose and need extracting. This severe form of gum disease is known as periodontitis which means inflammation around the tooth.
Indicators of gum disease to be aware of and to alert your health provider to:
-
Structural changes in your mouth such as bite, fit of teeth or in the fit of prosthetics (dentures) or tooth movement.
-
Pockets forming between the gums and teeth.
-
Red, swollen, sore or receding gums or gums that bleed.
-
Halitosis (bad breath) or dysgeusia (unpleasant taste in the mouth).
What can you do to manage problems, such as red, sore and bleeding gums arising from periodontal disease?
The key is, of course, good oral hygiene, involving:
- twice-daily brushing,
- regular flossing,
- use of antibacterial mouthwashes.
Underpinning suggestions above is a well-balanced diet, being well-hydrated and not smoking.
Treatments range from deep cleaning (often known as a scale and root plane) and medications to surgical treatment:
-
Dental (deep) cleaning. This involves removing the tartar from around the gum line (above and below) and root planing which removes abrasive spots on the root of the tooth, which is a place that bacteria can collect.
-
Antimicrobial mouthrinse on prescription. This contains an antimicrobial called chlorhexidine which is used to counteract bacteria in gingivitis and after gum surgery. This is used like an ordinary mouthwash.
-
Antiseptic chip. This is a small piece of chlorhexidine-filled gelatin which is placed in periodontal pockets after root planing; this is to facilitate slow-release of the medication to control the bacteria and reduce the size of periodontal pockets.
-
Antibiotic gel. This contains the antibiotic doxycycline and is inserted into pockets by the periodontist following scaling and root planing. Again, this is a slow-release medication (over a seven-day period) used to counteract bacteria and reduce the size of periodontal pockets.
-
Antibiotic microspheres. Here, the periodontist puts tiny spheres known as microspheres containing the antibiotic minocycline into the pockets after scaling and root planing, this is a slow-release medication, again used to control bacteria and reduce the size of periodontal pockets.
-
Enzyme suppressant This is a low dose of the medication doxycycline used to address destructive enzymes which if uncontrolled can break down gum tissue. It is prescribed in tablet form and designed for use in conjunction with scaling and root planing.
-
Oral antibiotics. These come in tablet or capsule form and are used to manage localized, acute infection over a short-term period.
-
Surgical treatment includes flap surgery and bone and tissue grafts.
-
Flap surgery involves removal of calculus in periodontal pockets or reduction of the pocket itself to make dental hygiene easier.
-
Bone and tissue grafts may also be suggested to restore damaged bone or tissue which has resulted from periodontitis.
-
Treatment may vary but all approaches will focus on controlling infection. Integral to treatment will be good oral hygiene practices which individuals are required to maintain independently, alongside more holistic approaches such as lifestyle change (diet, smoking etc.) to support treatment goals. Current advice is to visit your dentist once per year.


Your thoughts on this