Overview of scarlet fever (scarlatina)
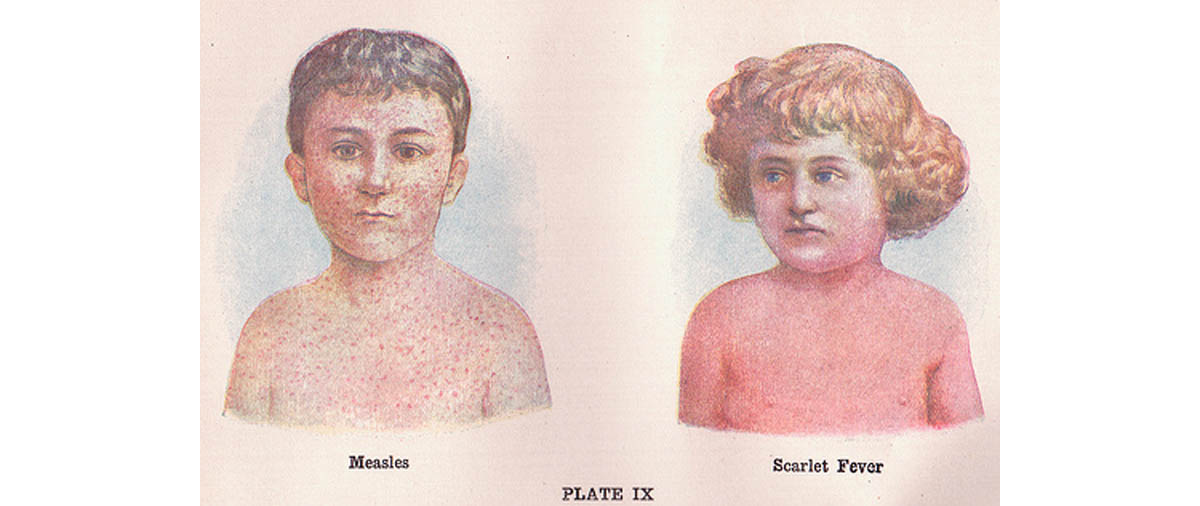
Scarlet fever is characterized by the presence of fever and generalized eruption of bright red points or small macules, along with other constitutional disturbances.
In general, scarlet fever develops from an upper respiratory infection such as a pharyngeal or tonsillar infection. Rarely, it may develop after streptococcal infection of the skin and soft tissue. The beta-hemolytic type A streptococci produces a number of erythrogenic toxins that cause the distinctive rash of scarlet fever. The bacteria survive extremes of temperature and humidity. Infection usually spreads through airborne respiratory particles transmitted from infected patients and asymptomatic carriers. The infection rate increases in overcrowded settings.
Once considered a serious disease with high rate of mortality and morbidity, today, scarlet fever infection is a less threatening condition as modern antibiotics play vital role to make the disease follow a benign course. If left untreated, the illness can sometimes lead to serious conditions affecting the heart and kidneys. The most common treatment for scarlet fever is a ten day course of antibiotics and it usually resolves without complications following early and appropriate treatment.
Scarlet fever clinical signs and characteristics of the Rash
Clinical Signs
Signs and symptoms of scarlet fever generally appear about 1 to 4 days after initial infection and these include the following:
- Sudden onset of fever with chills
- Sore throat with enlarged tonsils
- Nausea and vomiting
- Bright red sandpaper-like rash of 1 to 2 mm in size
- White coating on the tongue that later peels away leaving a red and swollen tongue, referred as strawberry tongue.
- General malaise
- Enlarged lymph nodes
- Loss of appetite
- Abdominal pain
Characteristics of the Rash
Typically, the rash consists of erythematous patches, initially appearing below the ears, chest and axilla, which later merge together and move to the trunk, arms and legs. The rash can be slightly itchy. Dissemination to the trunk and extremities occurs over 24 hours. It usually develops 12 to 48 hours after the onset of fever. As the rash become more diffuse, they punctate in the size of pinheads giving the skin rough sandpaper-like texture.
Rupture of the blood vessels at these sites is observed as linear arrays of petechiae known as Pastia lines which may remain for 1 to 2 days after disappearance of the rash. The eruptions generally persist for 4 to 6 days, gradually fading away, and are followed by a branny desquamation. The desquamation begins 7 to10 days after resolution of the rash and may continue up to 6 weeks. The skin becomes dry and is shed in the form of dry, bran-like scales.
Scarlet fever diagnosis, treatment and complications
Diagnosis
The diagnosis of scarlet fever can be straight away made from the appearance of the erythematous patches with the innumerable small red points. In addition, the presence of sore throat and the strawberry tongue are suggestive of scarlet fever. It is important to perform some tests to confirm the diagnosis. A culture swab taken from the throat is the standard criteria for confirmation of group A streptococcal upper respiratory infection. Direct antigen detection kits which tests the level of ASO, anti-streptolysin O (an antibody to streptolysin O) in the blood, allow immediate diagnosis and prompt administration of antibiotics.
Treatment
Majority cases of mild scarlet fever resolve within a week without treatment. However, appropriate treatment helps to accelerate the recovery and reduce the risk of complications.
The goals of treatment include the following:
- To shorten the course of illness
- To prevent acute rheumatic fever
- To reduce the spread of infection
- To prevent suppurative complications
While penicillin is the antibiotic of choice in the medical management of scarlet fever, a first-generation cephalosporin is an effective alternative, as long as the patient does not have anaphylactic reactions to penicillin. Amoxicillin, a derivative of penicillin and tastes better is a preferred antibiotic for children. Erythromycin can also be considered as an alternative.
A minimum of 24 hours of antibiotic therapy should be given and continued for 10 days before a child return to school in order to prevent the spread of the disease, as the child is no longer contagious after 24 hours of starting the antibiotics. Treatment is given for 10 days in order to prevent complications of rheumatic fever and rheumatic heart disease. Patients generally recover about 3 to 4 days after initiation of treatment.
Other aspects of treatment include the following:
- Increase fluid intake.
- Paracetamol helps to relieve fever, and pains.
- Calamine lotion can be applied to relieve skin itchiness.
- A salt water gargle may ease the throat pain.
Complications
Complications are rare with early and appropriate initiation of therapy. Nevertheless, the following complications are possible:
- Throat abscess
- Sinusitis
- Ear infection
- Bronchopneumonia
- Poststreptococcal glomerulonephritis
- Kidney damage
- Rheumatic fever
- Secondary skin infections
- Meningitis
- Brain abscess
- Endocarditis
- Osteomyelitis
- Hepatitis
- Toxic shock syndrome
Read More: Once An Almost-Forgotten Disease, Measles Outbreak Strikes Children And Adults
Prevention
The prevention strategies are the same as the standard precautions against infections. Some of the preventive measures are:
- Isolation – Keep the child isolated in a comfortable room.
- Handkerchiefs or tissues that the child used should be washed or disposed of immediately.
- Handwashing – teach the child to frequently wash his/her hands thoroughly.
- Coughing and sneezing - the child should be taught to cover his/her mouth and nose when coughing and sneezing.
- Do not allow the child to share drinking glasses or eating utensils.
- emedicine.medscape.com/article/785981-overview
- www.emedicinehealth.com/skin_rashes_in_children/page2_em.htm
- www.swsbm.com/EclecticMed/Eclectic%20Medicine_Part_Ib.pdf

