Overview
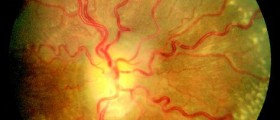
The increased pressure inside the head can result in swelling of the optic nerve and may lead to vision loss. Therefore, it is very important that the condition is managed in time and effectively enough to prevent such a complication from occurring.

Treatment Options
Medical
Reversible factors such as the weight of obese patients and any triggers that lead to an increase in intracranial pressure should be addressed.
In those patients who are not experiencing any issues with their vision are managed with Acetazolamide for six months coupled together with a sodium-restricted diet. According to the Idiopathic Intracranial Hypertension Trial, this therapy was proven to help reduce the intracranial pressure in affected individuals and improved their quality of life. Patients who didn't tolerate Acetazolamide were prescribed furosemide as a replacement diuretic medications, but it doesn't seem to be as effective as the former drug.
Patients who experience headaches but have a stable visual function can be managed with medications such as propranolol and amitryptiline, as well as any other commonly prescribed anti-migraine medications. One drug that has been used for its side effect of weight loss is topiramate and this helps to put the condition into remission.
In those who do experience any progressive visual loss in one or both eyes or if there is a poor response to the mentioned medication, a short course of high-dose oral steroids is prescribed and this helps to postpone any surgical intervention to address the pressure on the optic nerve. The steroids help to reduce any inflammation that may be causing the increased intracranial pressure.
Surgical
The two surgical options include optic nerve sheath fenestration and cerebrospinal fluid (CSF) diversion.
Optic sheath fenestration involves cutting into the dura tissue that surrounds the optic nerve located immediately behind the globe of the eye. This allows more space for the optic nerve so that it isn't compressed when the intracranial pressure rises.
CSF diversion involves performing a procedure known as ventriculoperitoneal shunting where a shunt is inserted in the ventricle of the brain, where CSF is produced, and the distal end is placed in the abdominal cavity. The excess CSF produced by the ventricle is diverted to the abdomen where it is absorbed and this helps to keep the intracranial pressure from elevating to abnormal levels.
Considerations
The exact time frame within which visual loss can be reversed after affected patients complain of such issues is not known. The opinions from experts in this field of medicine vary as to how quickly and aggressively affected patients should be treated.
- www.ncbi.nlm.nih.gov/pmc/articles/PMC2908600/
- Photo courtesy of SteadyHealth