Table of Contents
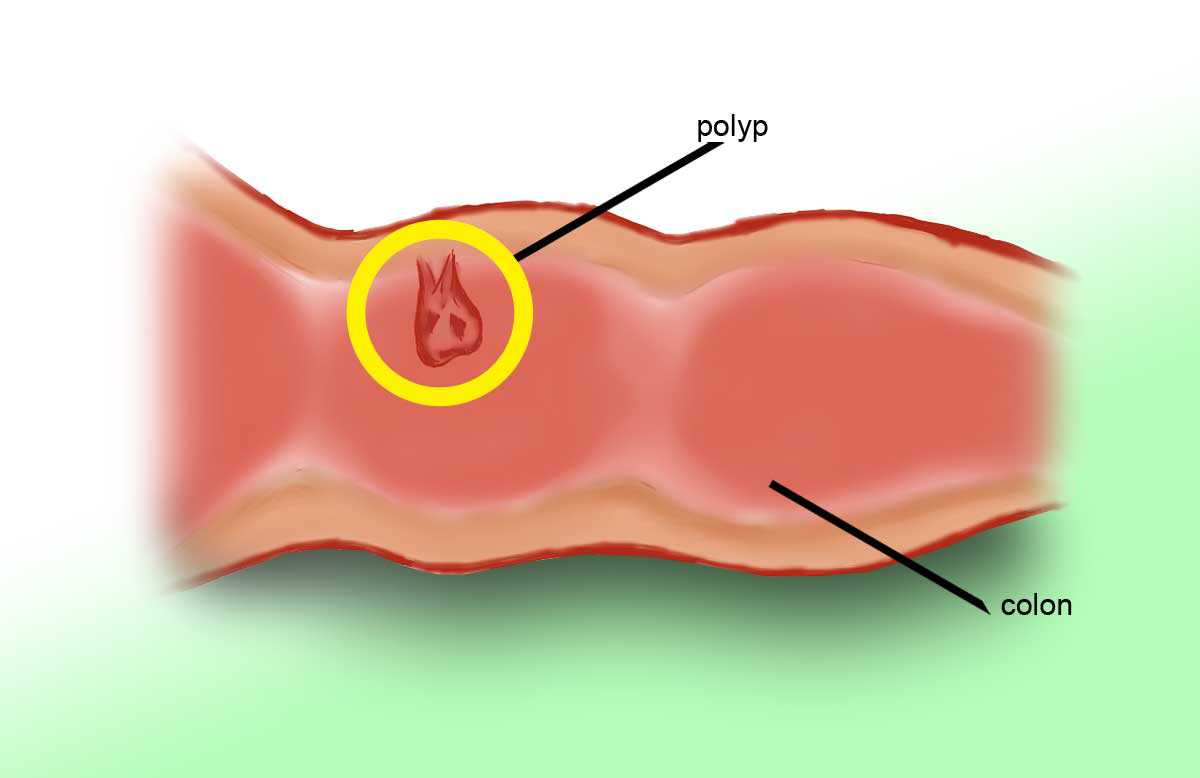
What are polyps?
Polyps are usually classified into two types: adenomatous polyps (adenomas) and hyperplastic polyps.
Most polyps are noncancerous and cause no symptoms. They are called hyperplastic polyps.
Adenomas are the precursor lesions for colorectal carcinoma (colon cancer). The more common hyperplastic polyps are benign and, in most circumstances, are not considered to be pre-malignant.
A colorectal polyp is a growth that sticks out of the lining of the colon or rectum. Polyps are grape-like growths on the lining of the colon and rectum, they can be single or multiple and do become more common in people over age 50. Usually colorectal polyps are benign, but when left untreated, they can in some cases slowly begin develop into cancer, a process that can take years, although the polyps still will not cause any symptoms.
Colorectal polyps are most of the time benign (meaning that they are not cancerous, not necessarily that they pose no danger at all), but these small growths may cause painless rectal bleeding in some people. Below we will discus types of colorectal polyps that have or don't have the tendency to become cancerous.
Polyps may be (besides age and family history) also associated with some hereditary disorders:
- Gardner's syndrome
- Peutz-Jeghers syndrome
- Lynch syndrome (HNPCC)
- Juvenile polyposis
- Familial adenomatous polyposis
Symptoms of Colorectal Polyps
Colorectal polyps do not cause any symptoms in the majority of cases; however, the following symptoms might occur in some patients:- bleeding from the rectum, which is painless
- bloody stool or any unusual changes in routine bowel movements
- abdominal pain
- fatigue and anemia
- unexplained weight loss
Are Colorectal Polyps cancerous or not?
Most types of polyps, also called hyperplastic polyps, do not have a tendency to develop into cancer. However, over time, certain types of polyps, also called adenomatous polyps, may develop into cancer. Also, polyps greater than one centimeter in diameter have a greater cancer risk associated with them than polyps sized under one centimeter in diameter. Risk factors for polyps developing into cancer include advancing age (over age 50) or a family history of colon cancer or polyps.Read More: Colorectal (Colon) Cancer: Causes, Symptoms and Treatment
Hyperplastic Polyps and Treatment Options
If only hyperplastic polyps are found during your flexible sigmoidoscopy, you usually do not need to have a colonoscopy.In some cases of very small polyps (5 mm or less) they may not be removed. Namely, some studies have concluded that even if they contain adenomatous tissue, these polyps take so many years to grow that they pose little risk of cancer. This is an exception in people who have inherited polyp syndromes. In their case the polyp will need to be removed.
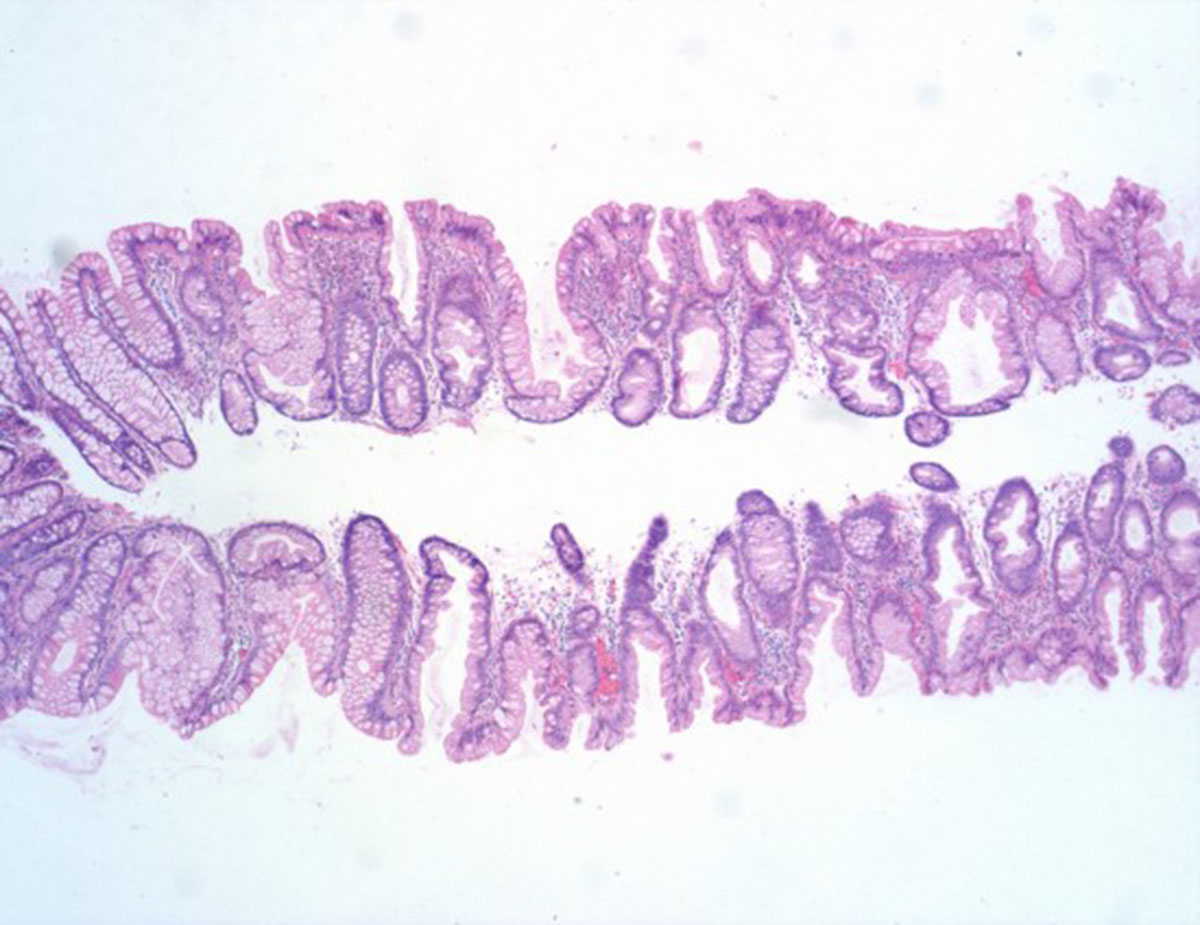
Adenomatous polyps (adenomas) of the colon and rectum are benign (non-cancerous) growths that have the potential to develop into colorectal cancer over time, or in other words, they are considered to be pre-malignant. Thus, colorectal adenomatous polyps (adenomas) can develop into cancer and they should be removed. They are larger than one centimeter and are associated with a greater risk of cancer. If they aren't removed, they continue to grow and eventually become cancerous.
Most larger polyps are adenomatous, nevertheless this must be determined by tissue examination, also called a biopsy. If during an exam with a flexible sigmoidoscopy adenomatous polyps are found, a colonoscopy is done to look for and remove any polyps in the rest of the colon.
- Puncturing the colon or causing severe bleeding by damaging the wall of the colon
- Bleeding caused by removing a polyp.
- Complications from sedatives given during the procedure.
For larger colon polyps that have a broad area of attachment to the colon wall surgery is needed. These large polyps often cannot be removed safely during a colonoscopy and may be more likely to develop into cancer.
Read More: Colon (Colorectal) Cancer: Risks and Prevention Tips
In conclusion
Regular screenings for colon polyps are the best way to prevent polyps from developing into colon cancer. All men and women ages 50 and older should have a fecal occult blood test every year, a flexible sigmoidoscopy every 5 years, or both. However, if you have had one or more adenomatous polyps removed, you probably need regular follow-up colonoscopy exams every few years.- www.webmd.com/colorectal-cancer/guide/colorectal-polyps-cancer
- www.cancer.org/docroot/CRI/content/CRI_2_4_3x_Can_Colon_and_rectum_cancer_be_found_early.asp
- picture: www.dnadirect.com
- Photo courtesy of Jeremy T. Hetzel by Flickr : www.flickr.com/photos/jthetzel/4318005626/

