Loading...
good luck to you
Loading...
Hi there. Well, everyone stool normally contains a small amount of mucus because it can make to keep the lining of your colon moist and lubricated. But if you notice some larger amounts of mucus in stool, that means that it be caused by certain intestinal infections Very often, it is normal to see a blood in stool after drinking - it happens to me once a month because I am not getting along with alcohol. It usually disappears after a day or maximum two days.Anyway, if you notice that this blood issue goes on, you should contact your doctor.
Loading...
Well, anyways, I noticed that you posted about 1 1/2 years ago...did you ever find anything out about this? Did it go away or are you still living with the problem?
Loading...
Loading...
Loading...
OK - my symptoms were:
Blood in stools, starting with a bit of bright red blood on the stool, then becoming part of the mucus that also appeared
Mucus in stools - quite noticeable
Some diarrhea - but nothing major
A bit of stomach rumbing
No real pain, possibly a bit of trapped wind pain, but nothing major
Went to the docs and he said, yeah probably piles. He checked me using a gloved finger and said that he couldn't feel or see anything - but this was not unusual for internal piles. He prescribed Anusol suppositories and Fibrogel to keep my stools soft (a bit odd as I had softish stools already). He took some blood tests just to be sure and said to come back in 2 weeks if things didn't improve.
After 2 weeks I had had a bit of improvement but I was still bleeding a bit and there was still mucus. The mucus was like a browny-red I'm assuming as a result of the delightful mixture of stool and blood. So I thought I should go back to see the doc. This time he said he still thought it was internal hemorrhoids and that the best thing would be for me to get checked out and if necessary I could get them injected, rather than continuing to bleed.
The blood tests were all normal - he'd tested for inflammation, celiac disease, liver and kidney function, thyroid function and anemia (I think).
I went to the clinic to get seen - they inserted a rigid tube into my backside - it wasn't painful but a little uncomfortable as they pump some air in. The doc said that it wasn't hemorrhoids and my colon was inflammed and bleeding quite a lot. She said that she couldn't really see properly and wanted to book me in for a flexible sigmoidoscopy (I think that's what its called).
I went back for the sigmoid thing and this time I had to have an enema before hand. They just pump some liquid up your bum and ask you to hold it in for 10 mins - which is quite hard! I lasted about 7 minutes :-)
Then the sigmoidoscope thing - you lay on your side and they put a flexible tube with a camera in it and you get to look at your colon on the TV screen. The sigmoidoscope just looks at the lower part of your colon - your rectum, the sigmoid colon and some of the descending (left-hadn side) colon. I could see my colon looked pretty red and the surface of it had tiny trails of blood - a bit like a very sore throat. I also saw some yellow ulcers (nice) and clear mucus. Amazingly there was no poop - I guess the enema did its job. She went as far as she could as the air that she had to pump in was making it a bit uncomfortable. So she wasn't able to see the extent of the inflammation.
She took a couple of biopsies (they kind of insert some sort of wire thing up the middle of the tube and it takes a little bit of tissue from inside the colon. You can't feel it at all.)
After that, she explained that I have ulcerative colitis. It's not super-mild, but it's not that bad either. It's kind of mild to moderate I think! If it was all the way up I think I would have more diarrhea etc.
That was just over a week ago and I have been taking some tablets called Pentasa (which contains Mesalazine) and a foam called Colifoam which you insert up your bum each day. My symptoms appear to have completely gone! Maybe still a bit of mucus, but very mild and haven't seen any blood. I'm sure it's still inflammed, but the drugs seem to be working for me.
Hopefully I can bring it under control and not have to worry too much about it. I only open my bowels once a day and have no pain whatsoever, so fingers crosssed.
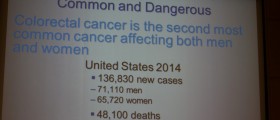
Although ulcerative colitis is a seroius condition and can elevate your risk of getting colon cancer, I am so relieved that I at least have a diagnosis because self-diagnosing online is a nightmare as you can never rule out cancer!
My advice would be for anyone experiencing similar symptoms, to not hang around - go to the Doctors - chances are its probably only piles, but even if it is something more serious it's better to get it looked at sooner because then you have a better chance of getting it treated. The process of being diagnosed is nothing to worry about - I was more worried about the outcome than the actual experience. OK, its not nice having someone stick a camera up your butt, but it's a quick procedure and worth it to know that you have done everything you need to.
I have yet to get the results of my biopsies - they take these to determine whether it is ulcerative colitis or Crohns disease. I think it is UC, just because of my symptoms and the fact they saw ulcers, but its good to get a proper diagnosis.
I hope this has been useful and that you all get back on the road to recovery as soon as possible!
Loading...
I have referred to this post many times in my search to understand what might be wrong with me. I never posted my symptoms because they are just what were described above. But, after having a colonoscopy today and receiving my results, I thought I would share. I was diagnosed with Ulcerative Colitis and Proctitis. It is not fatal, but not curable either.
***this post is edited by moderator *** *** web addresses not allowed*** Please read our Terms of Use
One more note, this is normally found in people between the ages of 15-30. Being 46, I am surprised to have something like this. Always knew I was "young at heart!" LOL
Good luck to all of you.
Loading...
Hi, I just wrote the above message. Start with eating 'soft' meats (as in ground meat, fish, homemade chicken soup), and slowly add VERY well cooked (almost mush) veggies. Rough or raw veggies or too hard on the lining of your colon, it's like eating glass! Get off all carbs (sugar) and eat well cooked 'soft' food until the bleeding stops...then buy the book and follow the rest of the diet! You can heal form UC!
Loading...
Not to be melodramatic, but I almost died from cross infections. Since I no longer respond to aggressive antibiotic treatment, I need surgery. The "normal" open procedure is very prone to problems of morbidity and mortality. After much research I have found a doctor that performs a totally laproscopic sigmoid colectomy. This gives many less problems and much faster recovery.
The long and the short of it is that you have to become very proactive about your own health. These symptoms should not be ignored, there is always a cause. Find a doctor that will get to the root of the problem!
Loading...
Loading...
Loading...
Loading...
I'm really lucky that may local hospital has one of the leading colo-rectal units in Europe based in it. My specialist thinks its colitis. Hopefully after this week I'll get a full diagnosis and start treatment.
Loading...
Loading...