Get a great colorectal surgeon! You will be fine ! As long as your core is strong, you will heal quickly. I was scared to death, but it's not so bad and after a year and a half I am free of pain and totally healed and happy with the choice I made. Best of luck!
Loading...
Went back to surgeon on the 26th for checkup. Told him my stools were still small and BMs were still a bit painful but not too bad. I wanted to go back to work so he ok'd it. He told me to start slowly adding more solid foods to my diet but avoid high fiber foods until after I see him again 3 weeks later.
Went back to work on Thurs the 28th and that's when things started going bad again. I realized that I had been having 3 or 4 BMs a day while at home and each one took a while of sitting in the bathroom. I couldn't do this at work (I've always had a hard time with BMs away from home but this was the worst ever - I just couldn't do it!) I had cut down to just one colace a day before this but now went up to 2 a day trying to have a BM at work. By Friday night (only my second day back at work) I felt miserably constipated and felt a lot of pain in the colon area, so I took a chance and ate a small helping of veggies. BIG MISTAKE. Saturday morning I was having excruciatingly painful BMs. Sunday was a little better but not much. Monday I went back to work and again felt a need to have a BM but couldn't do it. I took 2 colace that day also (but no more veggies). No BMs at work, but spent several painful hours in the bathroom that night.
Now it's Tuesday. I called in sick today. After my seventh painful BM this morning, I called my Dr. and he wanted me to go get some lab tests done (to check for infection I think?) I was about to go in but kept thinking about two things - not being able to BM at work and getting backed up from it, plus something about the colace - so I looked up colace and found out you're not supposed to take it more than one week. Prolonged use can cause constipation, diarrhea, pain in the peri-anal area and more. I was so sure that these two issues were my problem that I called my Doc back. I didn't get to talk to him but the nurse agreed with me and we've decided to let my bowel rest for two days at home, with no colace, and see if there's an improvement. Of course if I get worse or start running fever I will go to the hospital. (This also scares me a little because the initial infection I was hospitalized with had NO FEVER so how would I know if this is an infection?)
Bottom line - if you're going to have this surgery, do LOTS of research and ask LOTS of questions. Research every drug you take, even if it's over the counter. Find lists of safe foods to eat and foods to avoid (I finally did this, and found some contradicting info - I finally decided if ANYONE said it was bad, don't eat it.) As you get better, add new foods in ONE AT A TIME then wait to see if it agreed with you. And don't get in too big of a hurry to go back to work, especially if you normally have problems having a BM in public bathrooms like I do. I've talked to my boss about the problem (how embarrassing - discussing toilet habits with your boss?? wow) and we've decided that I'll just work half days until I KNOW I'm better. This way I'm not holding so much in my bowels when I get home from work.
Several posters mentioned everyone is different - HOW TRUE!! I would give my right arm to be able to eat a good salad or stir-fry, if I knew the pain wouldn't kill me, but I can't. I will post a follow up in a few days. Best wishes to all who have had or are soon to have this surgery.
Loading...
Loading...
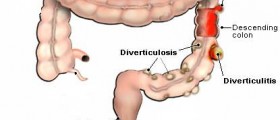
I was dianosed with diverticulitis at age 41. I've had 10 epasodes of this painful stuff and now I'm going to have it removed. I'm alittle nerveous. Just wondering with me waiting to long how much of the colon will have to be removed. Hopefully everything goes well. I'm so tiered of being bloated and looking like I'm pregant with twins. I'm exercising 4 days aweek so my surgery goes good.
Loading...
Loading...
Loading...
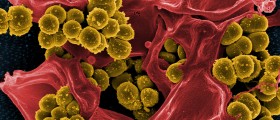
And I will repeat myself regarding c.diff - colon surgery puts you at higher risk for c.diff. if you get better after the surgery, then start getting worse, like I did, get tested for c.diff as soon as possible. I wish I had known about it sooner.
Loading...
Loading...
Anyway, ISSIE - please don't freak out. It takes 2 days for the antibiotics to START working. And if the infection is bad, he may not feel much better for a few days after that. Give it a few days.
And don't freak out on my post about all the pain after the surgery. I was guessing this or that was causing it, but I was wrong. It was a c.diff infection but because I was immuno-depressed (rheumatoid arthritis and the meds I take for it) I didn't run a fever so I didn't know it was an infection.
Most likely he will start feeling better in the next few days, then they will send him home on antibiotics and a limited diet. Follow the diet and don't add more than one new food per day, to see how he tolerates it.
After the colon surgery, the diet is very important for the first 2 weeks or so, then start adding new foods (one a day) and see how well he tolerates them. Most people get back to a normal diet pretty quickly, some have trouble with certain foods. it will probably be a long while before he tolerates high fiber foods, and he should probably avoid foods that cause diverticulitis symptoms for the rest of his life (high fat foods, small seeds, nuts).
Don't expect infection, but be on the lookout for it after the surgery and get medical attention immediately if he was getting better then starts getting worse. My biggest mistake was waiting too long when I did that.
Keep your spirits up, and his too. He needs your support now. We'll support you. Post back if you have any more questions or concerns. I keep an eye on this topic and will respond.
Loading...
Loading...
Hi I am 51 but I have been having problems with diverticutilits for about 12 years. I have had about 13 attacks each one getting worse til I was hospitalized in Mar than again in aug with an attack in july that i could stay in hospital due to obligations so they gave me iv meds n sent me home....I am due to have surgery Sept 27 n these post has helped my understanding of the surgery n after surgery....I am not getting the main surgery i am getting laposcopy surgery which i understand is alot less pain...will post my after surgery thoughts later....good luck to all of you
Loading...
Loading...
Just had the surgery an sorry to say it wasnt a pleasant ordeal. Be prepared to hurt, abdominal surgery is painful because it seems you use your stomach to do everything, im going on 3 months after surgery an still am tender. Try an not be scared of something you cant control, you will feel so much better once you get through the first part.
Loading...
HI, 49 and having lapra. on Nov. 5 . I've been having attacks since 2003. After 10 years of dealing with this disease, I'm scared of what they might find in there! I'm not so concerned with the pain aspect, but for how long the pain will be there. Xmas is just around the corner and as we all know , so are all the goodies.
Loading...
Are you getting only part of the large intestine removed or all? I have been through both. Part 10 years ago and all of it with a "J Pouch" (instead of the bag) 2 months ago. I recovered well with the first surgery. This last one has been hell. If you are getting part removed, follow a strict diet so that it does not reoccur as it did with me. I thought it was gone and could not come back, wrong! With this last surgery I was in the hospital 23 days, home for 10 days and back for another 7 as I could not eat, constant nausea and abdominal pain. 20 trips to the bathroom day and night. I have lost 15 lbs, down to 109 and still have problems with appetite. I have also become depressed over the lack of quality of my life, out of work for 2 months. I know it has only been 2 months but it seems much longer. I am praying that things will get much better soon, before I starve. Do your research, get a second opinion. Just be informed. I am over 50 so I probably will not heal as a younger person would.
Loading...