I had a LAR 18 months ago and have this problem. I mentioned it to the consultant during a routine check and she arranged tests to try and identify the cause and come up with a possible solution.
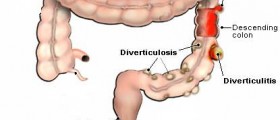
It turns out the cause is simple... they have removed the part of the bowel that does the squeezing and expels the waste during a BM, what happens now is that I can only expel what is sitting at the exit (making me feel like I need to go, and as soon as I leave the toilet gravity moves the next lot.. hence lots of trips to the toilet in an hour or two.
I have found the best way to deal with it for me is to use an enema before I go to work in the morning and I'm safe for the rest of the day.
The good news is, the surgeon says the bowel can 'learn' to squeeze over time, so it may get back to normal eventually.
Loading...
40 yr old male. Had my LAR 8.5 weeks ago. Cancerous polyp. 12 inches removed, 1 inch of rectum. Wow, I had a lack of respect for this procedure coming into it. I have had the lower pain a lot, tons of trips to the bathroom. In bunches. Dr said eat a bunch of fiber...I learned fast I cannot handle that. Caused constant bathroom trips and serious pain. I'm going to try the immodium as some have mentioned, hopefully will avoid the repeated trips each day. I called a week ago for some more pain meds and the nurse said if I want more I have to come see the surgeon. She acted as if I shouldn't need pain meds at this stage. Now I have read on here that many have pain months and years afterward. Not sure what to think. Tired of it. Dr said I could eat what I want...not the case. It is comforting to read that others have dealt with similar issues. Hope the thread continues.
Loading...
Dear yeargan, I had colon resection about six months ago. For about four months now I also have had pain in my bottom and rectum area. Have you gotten any help for your problem? I am needing some help. I have tried antispasmodic with no results. Bowel movements are not really an issue, but this pain is getting to me.
Loading...
I agree with your comments. I felt a bit out on a limb after a lower anterior resection and a temporary bag after I returned home after 12 days in hospital. I was told that I should feel alright after six weeks and to take a paracetamol for any pain you may have as if you had just had a tooth removed instead of a rectum. HUH. The pain got so bad I had to take oramorphine for three months, couldn't sit upright in a chair or car seat for three months without discomfort. Its now five months post-op the normal mucus and little faecal matter I pass always causes discomfort, take Cocodomol for that, worrying all the time about the amount of pain killers you have to take. I read one silly article saying you can have sexual intercourse three weeks post op, presumably running a marathon after six weeks. When people have to turn to the Web for information and with so much misinformation out there, then that is a bad state of affairs.
Loading...
Loading...
I had a low anterior resection in January 2014. Going to the bathroom only 8-9 times per day is great!!!! You will get used to it. You will figure out how to work around it. Trust me. All things are possible.
Loading...
I had a lower anterior resection to remove a colorectal cancer in 2011 followed by 2 months with a stoma and, after the reversal, 7 months of chemo. I too suffered the double digit trips to the toilet each day... usually involving repeated trips in rapid succession because within moments of each time I stood up afterward I felt the urge to go again.
Whilst everybody is different in terms of recovery from the surgery and recovery of anything resembling a normal bowel movement, I was advised that the part of my colon/rectum that 'squeezes' was removed hence the inability to evacuate normally. I was also told that over the coming months/years my body may 'learn' how to mimic that squeezing to allow more normal movements.
Following various attempts by my GP to improve and regulate things with laxatives and the like, I found that the best solution for me is 2 loperamide tablets (generic name of the active ingredient of imodium) each morning, after a cold water enema. It allows me to choose the time of the clearout depending on my shifts and I only have to do it once a day and, generally speaking, I don't have to avoid any foods. Occasionally I have to take more loperamide during a day if my diet or general wellbeing dictate.
Whilst I would love to regain full control (I do try now and again to see) I am content with the solution I have found, it works for me.
Try not to get despondent, particularly reading other peoples problems, they may or may not affect you the same, but do try all the alternatives... you should find one that suits your way of life. I personally detested the stoma and will do all I can to avoid that as a long term solution, but I also realise that for some that is the only, or preferred option.
I wish anyone well that has, or is about to go through it, stay strong and keep talking about it, whilst it often feels like it, you aren't alone.
Loading...
I was told in hospital to take paracetamol at home, something which I associate with a slight headache or toothache not for pain after my LAR surgery. The pain got worse after the first three weeks, nothing I took worked had to go on morphine in the end for three months then changed to Zapain which now works well for me. I had an Ileostomy reversal 7 months ago and still take pain killers when I have a flare up usually when I get constipated which is my norm and is another story. Only for the internet I would have felt very alone, they don't warn you in hospital, they don't have a clue what people go through unless they go through it themselves. I got more information from my specialist nurse at the oncology department who told me that many people who go through LAR have lower back pain and twinges at the side. Looking on the bright side I am doing well, and glad to be alive, but it does take time to recover from such an invasive operation.
Loading...
I had my LAR July 2013 followed by ileostomy reversal 6 months later. I too have experienced the burning bottom episodes like you have eaten too much chilli, thankfully my last one was few months ago so reckon it does clear up in time, but I do drink loads of water and try keep my body hydrated.
Loading...
I found your comment very helpful other comments such as feeling normal after a few months (lucky them) made me feel like there was something wrong with me. Had LAR 15 months ago ileostomy reversal nearly 9 months ago but still go to the toilet lots of times a day and constipation is the biggest problem and the lower back pain is still with me, guess after your rectum is removed the padding there is gone too and you feel discomfort in that area especially when you need to empty what is left of your bowels. Agree about surgeons they are very good at what they do but afterwards mine seemed surprised that I was having any issues at all.
Loading...
I recently had a LAR,six weeks ago and since then I have had pain in the rectum area which means I cannot sit down.
I know this is an old post, is there a recent site / forum I can visit?
Loading...
Look under "Body & Health Conditions / Gastrointestinal Disorders / Intestinal Problems & Bowel Movements" or search 'colon resection' or just start a new topic. I have had LAR, and know of an older woman who had problems sitting down after LAR.
Loading...
I am 3 years post lower anterior resection due to rectal cancer. What you all are experiencing is LARS (lower anterior resection syndrome). It's real and it can be very difficult. I have it but it is manageable for me. It sounds like some have it worse than others. I will say that it did improve a little for me over time. Or maybe I just have adapted. I have never had pain except for the irritation that occurs with chronic diahrrea. But wipes and A&D ointment prevent that. My system is now inconsistent. Sometimes I am constipated and sometimes I go frequently (6-10 times per day). I think much depends on diet however I have yet to figure out what I should eat to make it more consistent. I either go to little or too much. There is info on the internet about the Syndrome that gives suggestions as to how to manage it. Where I live we actually have a Colorectal Support Group that meets once per month. It is facilitated by a nurse and we have guest speakers that tend to be professionals in the field. I can see where this syndrome can be very disabling for some people. I hope for the best for all of you!
Loading...
Loading...
Well, I'm not really sure how to begin this post. Have never posted on any sites, ever, for anything. BUT.... Nine months ago had lower sigmoid colectomy/anamastosis for stage 1 colon cancer, which, despite minimal sub-mucosal invasion, was confined to a polyp found and removed during routine colonoscopy. My NH GI referred to local surgeon, who explained necessary procedure. Went to Boston for 2nd opinion - from path. slides, oncologist saw no further lymph invasion. Was confused, as I went to Boston because that's where I preferred to have surgery done. So, finally decided to get 3rd Boston opinion. Looking at same slides, this onco. said was definite invasion beyond original site, and that surgery a must. Surgery "went well".....but my life has been hellish, since. Don't want to take up too much space, but I assumed that at this point things would have 'normalized' somewhat. Incredible pressure/urgency/spasms, (like labor, for those of you who might be women); still quite frequent (up to 10/day) movements - and VERY compromised quality of life. Am much better if/when I don't eat, but....sort of a necessity. WHAT I eat makes no difference - (have always eaten carefully/healthily) - further sigmoidoscopy dx'd stricture w inflammation at connection site, and a few rounds of Canasa suppositories helped, but only temporarily. Am quite discouraged- especially because need to work, and at this point do not eat much at all while in office (am self-employed, so luckily have flexibility). On average, am in bathroom for several hrs/day, often until wee hrs. of morning -moaning in pain, and waiting to feel "emptied". Have been told (not by surgical or medical professionals, but by other surgical patients) that return to "normal" often takes up to a year. Sure wish I had known this prior to surgical procedure, as am not sure would have done it -especially since all 19 nodes removed along w 12" of colon, were "free and clear". First Boston doc, said no surgery (as risks greater than benefits), but recommended follow-up colonoscooy x 1 yr. In retrospect, wish I'd gone w his advice. This has been life-changing/altering....but am hoping that in another few months, things will have settled a bit more. For those of you who are only wks or even months out from surgery - hang in. And, you're correct, surgeons, regardless of how 'good' or well- trained and reputationed, do their job and refer back to GI docs to attempt clean-up. Good luck all. And don't be afraid (or intimidated) to get a second, or even third opinion. [Hopefully the opinions will coincide.] I did a lot of research prior to opting for surgery - and if I'd truly listened to my gut, and believed what my GI doc. told me post-colonoscopy ("I think I got it all" w polypectomy), I'd be a much happier camper right about now. The ONLY plus (and it doesn't even really count in the grand scheme of all the agony that has accompanied it, is that I lost 20# - so I 'feel' a little more comfortable (was not overweight, but outside world clothing feels more comfy....) an absolute miniscule consolation, however. This whole experience basically has been the pits. Am tired of complaining, of not knowing how to proceed, of wanting to regain some semblance of formerly active life - and at least know what the new "normal" will be, as the current one has been horrifically limiting. Time to 'hang-up'! Hope this has been somewhat helpful and not just a public whine.....take good care all....and please feel free to respond/ask questions.
Loading...