By the time you get into Biology 2 or the start of Organic Chemistry, chances are that you are gearing up towards your preparation for starting Medical School. You have heard from family and friends that it is paramount to get into a research project as soon as possible and you should be volunteering every free chance you get. Through all this chaos, you may have come across the acronyms DO and MD. These can be confusing points and as you shadow through hospitals, attending physicians may ask you if you are considering allopathic or osteopathic medicine and if you do not know the fundamental differences, you could be answering the questions all wrong. Some may have a vague understanding and know that "the MD is the desirable degree while a DO is an easier course," but unfortunately, there is no great differential to know if one degree prepares you better for a course in Medicine. In this article, I will cover some of the fundamental similarities and differences between the two degrees and then give you some insight into how patients will actually respond to each type of doctor when they enter the examining room.

Defining the Terms: What is an MD and DO degree?
Before we start our exploration into the field, it is important to understand the fundamental aim of each of these professions. An MD degree stands for Doctor of Medicine and is synonymous with the term "allopathic doctor." This profession is based on the fundamental idea that a sick patient will respond differently to a treatment than a healthy patient. For example, an antibiotic will not alter the health of a healthy patient while may vastly improve the health of an ill patient.
Now we come to the DO degree. This stands for Doctor of Osteopathic Medicine and it differs in the fundamental idea of how to treat a patient. These physicians train under a more holistic approach to the patient. When considering a disease, physicians with a DO background will consider the environment a patient lives in, his predisposing factors, and nutritional status in order maximize a patients response to therapy. Pain in the lower back could lead to muscle manipulation of the knees, hips, and chest in order to re-balance a patient. Now that we covered that, let's get started on the real material.
Similarities Between an MD and DO degree
One of the most important things to realize between a DO and MD degree is that they are both fully-licensed doctors. Both types of doctors are highly qualified and will be able to make the same difficult decisions in patient management. You are able to prescribe the same types of medications to the patients and you will be able to experience the same joy of drowning in paperwork when the hospital administration gets involved. A physician from both of these fields must complete the same 4-years of medical training and their residency programs in order to get licensed. With one of the two types of degrees, a physician will be able to practice medicine anywhere in the United States and they will have access to the same specializations if they qualify.
When you enter a hospital, patients really do not care where your degree is from as long as you are able to fully treat the patient. In reality, most patients actually think the DO on the doctor's ID badge is short for "Doctor" so they will not question your training once you begin practicing. As the training for DO programs improves, they are as skilled as their MD counterparts so the once popular saying that "good DO doctors are about as skilled as a bad MD doctor" is entirely false.
Why a DO Degree May Limit Your Opportunities in Medicine
Differences Between an MD and DO Degree
To get an MD degree, a medical student must be accepted to a Medical School accredited by the Liaison Committee on Medical Education (LCME) and he can do this by scoring high on the MCAT exam. An MCAT score of 31.4 corresponds to the average score that students will be accepted to after applying. This program is a 4-year program and during this process, a student must pass 3 different licensing exams in order to be able to begin Residency in a US program. These exams are referred to as STEP 1, STEP 2 Clinical Knowledge, and STEP 2 Clinical Skills. Once a student is accepted into a Residency Program, he will be able to apply for and take his final licensing examination referred to as STEP 3. These exams test a physicians understanding of the medical material the he has learned in school and the score that a candidate gets on the exam corresponds to the type of residency that a student will be able to apply to. In the United States, 67.4% of all currently practicing physicians are MDs. Due to their high scores on exams, MD doctors are usually the specialists in the hospital setting.
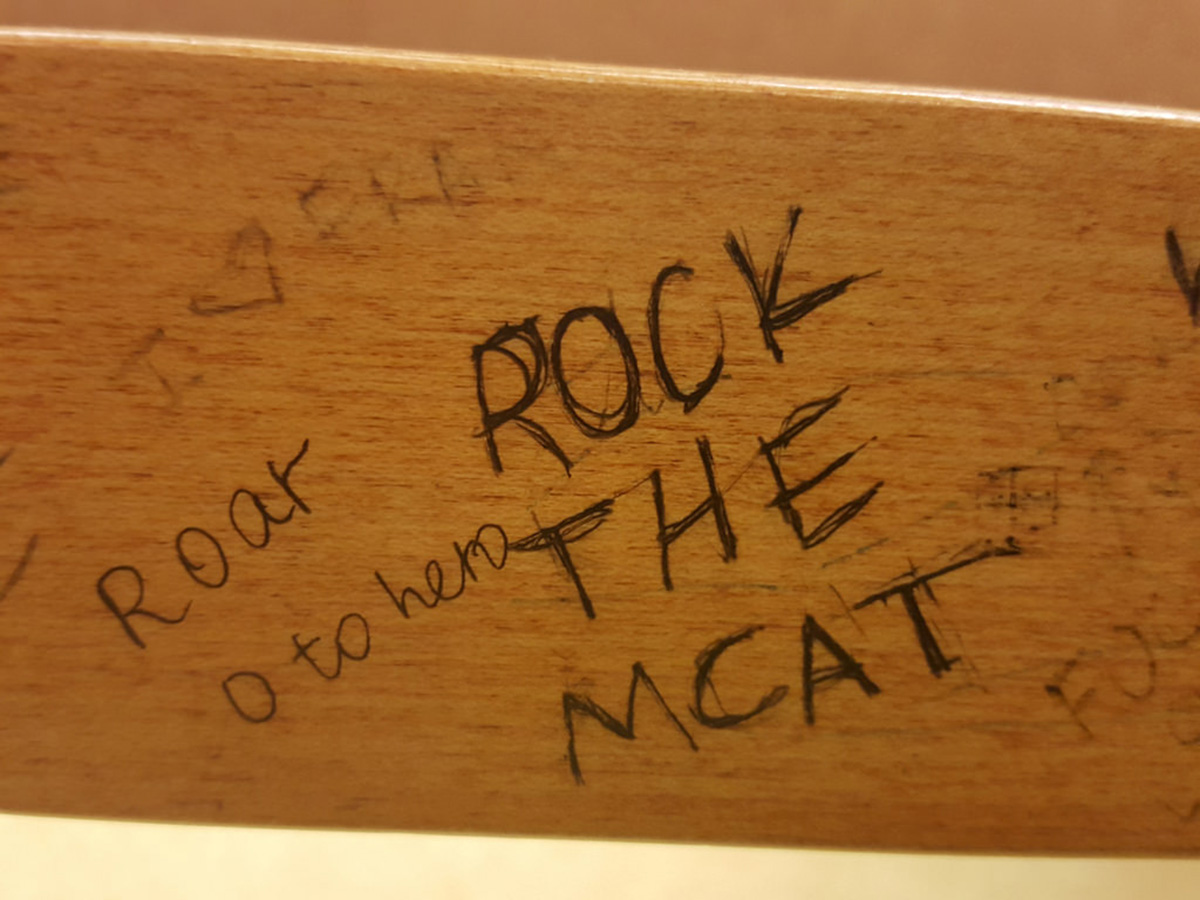
To get a DO degree, a medical student must take the MCAT exam and may not do as well as their MD counterparts. The average score to get into a DO program on the MCAT is 25.31. This program is also a 4-year program and during this process, a student faces 3 similar exams to STEP but these are called the COMLEX exams. Additionally, the student is required to learn 200 additional hours of manipulative training to learn how to treat musculoskeletal pain syndromes. The scores on these exams correspond to the type of specialty that a doctor can apply to. In the United States, 7.3% of all physicians hold a DO title. These doctors often find themselves in Family Medicine, Pediatrics, and Internal Medicine which are traditionally not as competitive as some of the more complex specialties like Dermatology, Ophthalmology, and Urology.
In terms of quality, it is getting harder and harder to tell the difference between a DO and an MD doctor in the hospital setting. More and more doctors are entering the wards as DOs and as their schooling improves, their training has become quite strong.
In my opinion, MDs could benefit from treating patients with more of a DO-approach. Often times, you find that patients have some type of lifestyle choice or perhaps an accident that happened 20 years ago that could be a key component of their pain currently. If MDs would consider that in managing patients, patients may not leave hospitals with 20 prescriptions for medications treating preexisting conditions. As hospitals become more blending, maybe this exchange of knowledge will gradually happen as the two work side-by-side and the patients will reap the benefits of two styles of medicine.
- 1.) http://myheart.net/articles/md-vs-do/
- Photo courtesy of shutterstock.com
- Photo courtesy of quinnanya: www.flickr.com/photos/quinnanya/25415605590/
- Photo courtesy of www.ilmicrofono.it: www.flickr.com/photos/115089924@N02/16070083419/

