The ovaries are the only female body part that literally "retires" when you cross into middle age. Ovarian function gradually starts declining as you enter the perimenopause, and eventually stops completely.
A menopausal state only can be declared if you have not menstruated for last one year. The average menopausal age of US women is at 51 years, with a most common age range of 48-55 years.
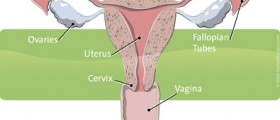
During reproductive age, the ovaries produce female hormones along with eggs. A gradual slowing of this hormonal production leads to some changes in mood, body, sleep and of course the menstrual cycle.
The menstrual cycle will lose its predictable cyclical pattern during the perimenopause. You may face scanty bleeding, irregular bleeding, long cycles, spotting and even heavy bleeding. These things are all normal.

The perimenopause doesn't always proceed in a straightforward manner, however, and there are diseases that produce similar symptoms. How do you differentiate between normal, physiological perimenopausal bleeding and pathological bleeding, then?
You should inform your clinician if you experience any of the following abnormal bleeding patterns while in the perimenopause:
- Heavy bleeding, especially with clots (requiring a pad every hour or need to change pads at night)
- Bleeding after sex
- Spotting or bleeding in between periods
- Cycles shorter than 21 days
- Periods lasting more than eight days
- Bleeding after attaining menopause
Apart from perimenopausal hormonal changes, an abnormal bleeding in the transitional period could also be the result of thyroid problems, chronic diseases, pelvic infection, fibroids, and uterine polyps or due to a potentially precancerous condition called endometrial hyperplasia.
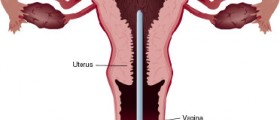
You need to undergo an evaluation to rule these conditions out if you experience the aforementioned symptoms. Various tests are available to assess your cycle status as well as to find any underlying pathology. Apart from a clinical examination, an ultrasound of the lower abdomen and a saline infusion sonohysterography are the two tests most often performed to assess the condition of your uterus and your endometrial thickness.
In special circumstances, you may need an endometrial biopsy to rule out any evidence of cancer. An endometrial biopsy is a minimally invasive option for endometrial evaluation in women at risk of malignancy.
You may need medical management when you are bleeding profusely, but do not suffer from any significant pathology. Combined oral contraceptive pills, cyclical oral or an injectable progesterone therapy, and a hormone emitting intrauterine device called the ‘’Mirena’’ are a few of the available options.
A hysterectomy (surgery to remove the uterus) may be needed when investigations reveal any uterine fibroid or polyp or any atypical endometrium that has a cancerous potential, or even when excessive bleeding cannot be controlled using the above medical management. However, an endometrial ablation may be a very good alternative. An endometrial ablation is a minimally invasive approach that recently became available and can replaces hysterectomy in some cases. During the procedure, the lining of the uterus is ablated to seal up blood vessels, something that thins the endometrium and often puts a stop to profuse bleeding.
In conclusion, irregular bleeding patterns during perimenopausal period are not always physiological. You have to be vigilant, as it may be caused by uterine polyps, tumors or even cancers and thus often needs an extensive evaluation.
- Photo courtesy of SteadyHealth