Loading...
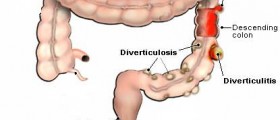
So I had a bowel resection (ileostomy & reversal) done in 2018 because of perforated bowels and I figured the pain I had would disappear with the affected bowel. It did not. When I told my GI about the pain he offered no testing but said it was muscle spasms. Muscle Spasms??!!!! That seems way too far fetched. Years later I am still having that pain at the site where bowels used to be. Every once in awhile I panicked thinking there were new perforations BUT I massaged the area last night and it did NOT activate my bowels like if I would have massaged my middle or left side abdomen. This let me know that the pain is not intestinal! And after reading so many comments here, I'm CONVINCED it's Phantom "Limb" Pain. Only when does it stop? Will it stop? What can be done?
Loading...
Loading...
Yes, all that pain medication was administered scheduled and daily. I STILL had pain, though I didn’t know my name. There were other mishaps,
But I was released after 35 days later: (unbelievably the liteny of pain medication was prescribed upon discharge; I was referred to pain management within two weeks. Instead of tapering me, she increased the meds.
I’ve had intense pain, daily, ever since. I’ve been to a few GI doctors who do not appear concerned. I’m concerned! I often have breath taking cramps to the point I pass out on the bathroom floor. I’ve been passing bright blood in my stool ever since the surgery. The original surgeon, who thought I was a joke, wrote my pain off, prescribed Metamucil, though I tried to explain that wasn’t the issue. Two years later, I had my gallbladder removed and gained 75 lbs. though I watched every calorie post-op. I’ve been scheduled for several colonoscopies, but the prep never works completely regardless how early I begin, the different type of prep, or days/weeks I set aside. My original scar area from the resection has enlarged, opened, and weeps. I suffering daily. I’m hoping anyone else can share or offer advice. I finally found a doc to take me off the pain medication, years ago. Unfortunately, I cannot find the help I need. I fear a true medical emergency. Additionally, I’ve tried to obtain my surgery report and records from my admission from the day I was release. It has disappeared from medical records.
Loading...
Loading...
Loading...