Surgery of the bowel involves removing or repairing diseased portions of the small or large intestine. The surgeon discusses all your options with you before proceeding with the operation. However, every surgery has its risks and complications, and if these manifest post-op, you should be prepared to deal with them effectively.
What Is Colorectal Surgery?
Diseases of the lower digestive tract, such as diverticulitis, hernia and inflammatory bowel disease (IBD), can cause parts of the tract to become infected. Injury and ischemia (restricted blood flow) can also cause damage to the affected areas. Obstructions within the rectum, due to scar tissue and other masses, can restrict the elimination of feces and produce sepsis. Colorectal surgery is performed to repair or remove such damaged or diseased sections of the colon, rectum, anus and sometimes even the pelvic floor.
What Does Colorectal Surgery For Cancer Involve?
Colorectal Surgery is a necessary course of action for people diagnosed with colorectal cancer. It usually results in major reconstruction of the lower intestinal tract. The procedure mainly involves removing any cancerous growths, repairing tears, removing blockages, and treating disorders of the pelvic floor.
Types Of Colorectal Surgery For Cancer
The type of surgery you have ultimately determines, to some extent, the type of complications you may develop. With advances in surgical treatments and techniques, there are various procedures available to perform colorectal surgery. Surgery depends on the location and type of cancer, and whether it has metastasized or not. There are two main types of surgeries:
- Open Surgery
- Endoscopic Surgery
Open Surgery – A Highly Invasive And Traditional Method
This involves making a large incision in the intestinal cavity to perform different types of repairs, such as a:
- Local Excision – cutting out very small early stage tumors without cutting through the abdominal wall.
- Resection and Anastomosis– the damaged section is cut out and the ends of the healthy section are stitched together; performed to remove early stage tumor and small tumors.
- Ostomy – creating an opening or a hole (stoma) inside the body which drains feces and urine into an external pouch (colostomy or ileostomy).
Endoscopic Surgery – Minimally Invasive and Modern
Instead of giving a large incision, the surgeon inserts a laparoscope (thin tube with a camera attached at one end) and other surgical instruments into the abdominal cavity via small incisions. This procedure has fewer chances of complications, a faster recovery rate, and minimal scarring. However, laparoscopic surgery is avoided in certain cases, such as very large tumors or other risk factors.
More often than not, patients experience immediate relief, and more than 90 percent do not develop a recurring problem. However, each individual and each surgery is different, and so are the expectations and possible outcomes.
Bowel Cancer Operation: Managing Post-Op Complications And Recovery
Complete recovery from colorectal surgery for cancer can take at least two to six weeks. Nevertheless, the exact duration of your healing depends on the type of surgical intervention, your individual characteristics and health status, and any existing medical conditions.

Physiological Complications
If you develop post-op complications, your recovery may take even longer than expected. The following section lists some of the typical things to watch out for after your colorectal surgery.
Wound Healing And Hygiene
Removal of the staples or stitches takes place at the hospital, or after a week or two following your surgery. Some stitches seal the wound inside the skin and dissolve on their own. Any steri-strips that are covering the wound will eventually fall off on their own accord. A little bruising is normal and improves with time. Keeping the site of the incision clean is also of primary importance. You must keep any dressings covering the wound dry to avoid the risk of getting it infected. Once the dressing is removed, wash the incision gently with soap and water, and if the wound is healing, you can shower after about 2 days as well.
Physical Activity
It takes about 3 months to regain complete physical fitness after colorectal surgery. It is normal to feel weak and exhausted when you leave the hospital. You have had a major surgery and the body needs time to regain its strength. You can be helped out of bed and into a chair at least a day after your surgery. Walking slowly in the hallway on the second day of surgery helps reduce the risks of developing blood clots and infection, and most of all, helps you get back the physical and psychological strength to stand on your own two feet.
Once back home, avoid heavy lifting and stick to light household chores. Indulge in short periods of reasonable physical work and take frequent breaks in between. Go for a moderate walk daily, and steadily increase the time and pace. Start your daily exercise regimes after consulting with a doctor. Avoid driving for at least two weeks after your surgery, especially if you are taking analgesics or any narcotics.
Nutritional Guidelines
Most people experience diarrhea and flatulence after surgery. A balanced diet and plenty of fluids are essential to keep you well nourished and hydrated. Eat small frequent meals to help your bowel resume its normal functioning again. It is important that you understand what foods suit you in your stages of recovery and consume those; the same diet does not apply to everyone.
If you experience severe abdominal pain and an inability to pass stool or wind, contact your doctor right away. On the contrary, do not ignore vomiting and persistent diarrhea as well, since these are indicative of adhesions and abdominal obstructions or infections. A prescription of stool softeners and antibiotics by your doctor will help.
Managing Pain
Some extent of abdominal discomfort from the wound or from passing wind is normal. The situation most often improves over several weeks. Keep taking the pain relieving drugs prescribed by your doctor until you feel at ease. Supporting your abdomen with a cushion and avoiding straining movements can help as well.
Sexual Intercourse
A physically demanding surgery will naturally affect your sex drive.
These symptoms are usually temporary and you can resume your sexual activities when you feel sufficiently comfortable. However, if they persist, consult your doctor.
Return to Work
If your job is of a sedentary nature, you can resume within two weeks. For a more physically demanding job, consider residual fatigue and take at least four to six weeks to rest.
Follow-up
Lifetime follow-ups are necessary after surgery to manage complications as they come and to aid recovery. They also help adjust medication and determine any relapses.
READ Chemotherapy For Colorectal Cancer
Psychological Complications
An impact that is not generally considered is the psychological effect of such a surgical procedure. You might have reservations regarding wearing a colostomy bag. You might develop symptoms of depression from the changes in lifestyle and appearance. A reduced sex drive and a fear of feeling sexually unappealing to your spouse is also common. In such cases, individual and family-oriented post-op counseling becomes essential in the recovery process.
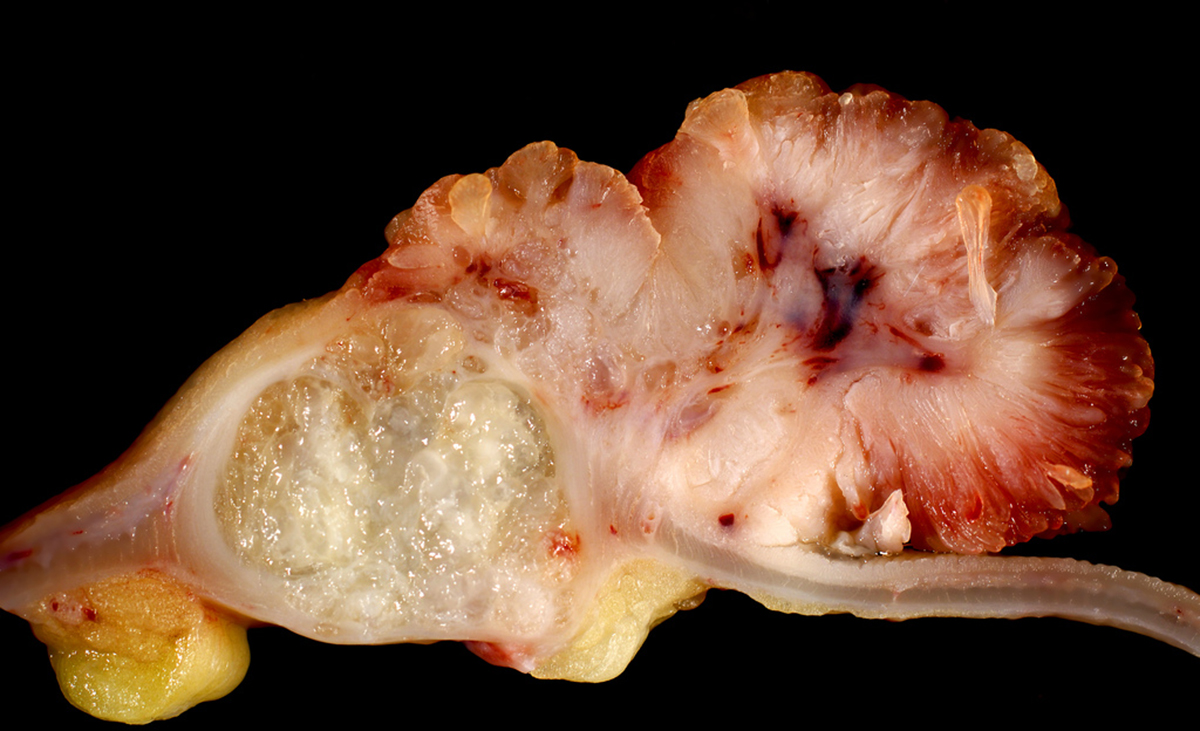
- Photo courtesy of euthman via Flickr: www.flickr.com/photos/euthman/438990160
- Photo courtesy of euthman via Flickr: www.flickr.com/photos/euthman/438990160
- Photo courtesy of Jimee, Jackie, Tom & Asha via Flickr: www.flickr.com/photos/wilderdom/221903845
- cmis.osu.edu/patient-care/colon/lapcolorectal/
- http://www.surgeryencyclopedia.com/Ce-Fi/Colorectal-Surgery.html
- http://www.jjs.me.uk/patientinfo/advicebowelsurgery.html

